This post was originally published on this site
A researcher slips stickers under some colored cups on a lazy Susan, then gives the tray a whirl. When the spinning stops, a preschooler must find the hidden stickers. Most children remember where the stickers are, but a few have to check every single cup.
The game tests working memory, which is among the set of mental skills known as executive function that can be impaired in children who faced trauma early in life.
Adversity wreaks havoc, and from there, “you have a system that responds differently,” says Megan Gunnar, a developmental psychobiologist at the University of Minnesota in Minneapolis who has spent two decades studying the impact of early-life adversity in adopted children. The focus of this work is extreme adversity, such as being orphaned, rather than everyday challenges, which might teach beneficial resilience.
A childhood characterized by hardship, negligence or abuse can also alter the neuroendocrine system that regulates how the body responds to stress. Problems in the stress response can set kids on a path toward behavior struggles along with increased risk for depression, diabetes and a host of other health problems.
But recent studies offer hints that such a difficult future may not be inevitable. As Gunnar and others have shown, impaired stress responses can return to normal during puberty, raising the possibility that imbalances created by early trauma can be erased. The research is prompting a new view of puberty as an opportunity — a chance for people who had a shaky start to reset their physiological responses to stress.
A sense of safety
When the brain perceives a threat — even a temporary one such as a stressful exam or a high-stakes competition — levels of the hormone adrenaline shoot up, setting off the “fight-or-flight” reaction. Breathing and heart rate soar. Palms get sweaty. Sight and other senses sharpen. Before long, the brain sends chemical messengers to stimulate adrenal glands near the kidneys to release cortisol.

Cortisol sends sugars into the blood for quick energy. The hormone also slows digestion, immune responses, growth and other processes considered nonessential in a fight-or-flight situation.
When the threat passes, the fight-or-flight response ends, at least in a person whose stress response is working as it should. Adrenaline and cortisol levels fall, heart rate slows and other systems resume business as usual.
When Gunnar started her doctoral work in the 1970s, researchers had already mapped out the key actors in the stress response. The neuro-endocrine signals involved form the HPA axis, short for hypothalamic-pituitary-adrenal. When rodents and monkeys face early-life adversity, the HPA axis gets thrown off-kilter. As methods became available for measuring cortisol from samples of saliva — rather than having to collect blood or urine — Gunnar set out to study how the HPA axis influences the brain and behavior in humans.
From experiments with newborn babies in the mid-1980s, Gunnar showed that having a secure parent relationship is important for a healthy neuroendocrine system and helps babies deal with stressful situations, such as getting immunizations. “You can go to the doctor as a baby and get a big shot in one leg and the other leg, and you’re crying your head off … but [the HPA axis] doesn’t kick off,” Gunnar says. However, shots or no shots, if babies get separated from their parents for even a few minutes, “their HPA axis shoots up like a rocket.”
Gunnar wondered what happens if that sense of safety is disrupted longer-term. She tried studying maltreated and impoverished children, but separating the effects of early hardship from later difficulties is not easy. “The way you start out in life tends to continue,” Gunnar says. A report published last November by the U.S. Centers for Disease Control and Prevention points to the long-term consequences: Compared with their peers, adults who experienced childhood trauma are more likely to smoke, drink heavily, have dropped out of high school and develop heart disease and a host of other chronic conditions.
A trip in the mid-1990s set Gunnar on a new path to answer that tricky research question. She ventured with a research team to an orphanage in eastern Romania, where young children were raised in overcrowded, inhumane conditions. “You walk into these wards, and all of a sudden you’re mobbed by kids saying ‘Mama, mama, mama’ … reaching their arms up to get held,” says Gunnar, who had two school-age sons at the time. “It was awful. I just wanted to bring them all home.”
What she did bring back to Minnesota, along with that searing memory, was a set of small vials, each containing a saliva sample from a 2- or 3-year-old orphan. To her surprise, the children’s cortisol levels — the end product of the neuroendocrine cascade — were lower than the average toddler’s. That finding offered a window into the effects of long-term parental deprivation on stress responses.
Adoptee struggles
To single out the effects of early hardship, Gunnar needed children who had started life in deprivation but then moved into healthy, supportive environments after infancy. Such children would be the ideal human analog for all of the animal studies on early adversity, she thought. It dawned on her that this group exists: adopted orphans.
Gunnar shared her idea with members of the adoption unit at the Minnesota Department of Human Services. With the department’s support and funding, she surveyed Minnesota parents who had adopted children internationally in the 1990s, and invited families to join a university registry and participate in research.
Many parents in the study had noticed early on that their adopted children had behavioral problems. And when the youngsters came to the university lab for problem-solving and sorting tests, including the lazy Susan task and the famous marshmallow test of delayed gratification (SN: 8/4/18, p. 14), the children struggled with attention and self-regulation.
Like the Romanian orphans, these kids had lower cortisol levels than nonadopted children who had no behavioral problems. In the face of sustained hardship, which has the potential to encourage dangerously high levels of cortisol, a weak stress response — that is, producing less cortisol — could be “nature’s way of preserving the brain and body,” Gunnar speculates.
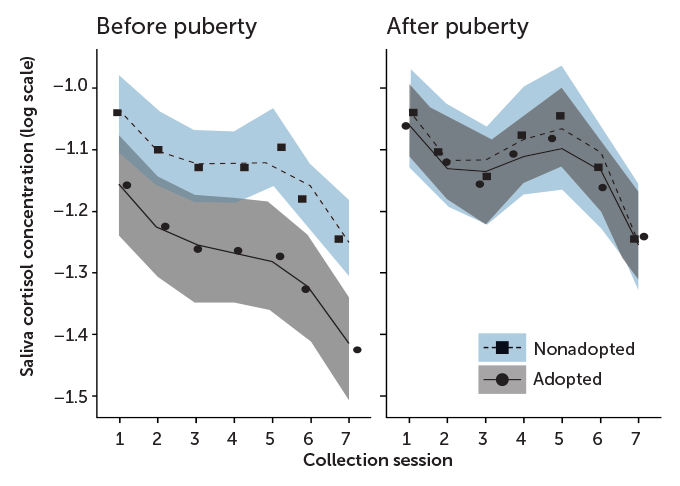
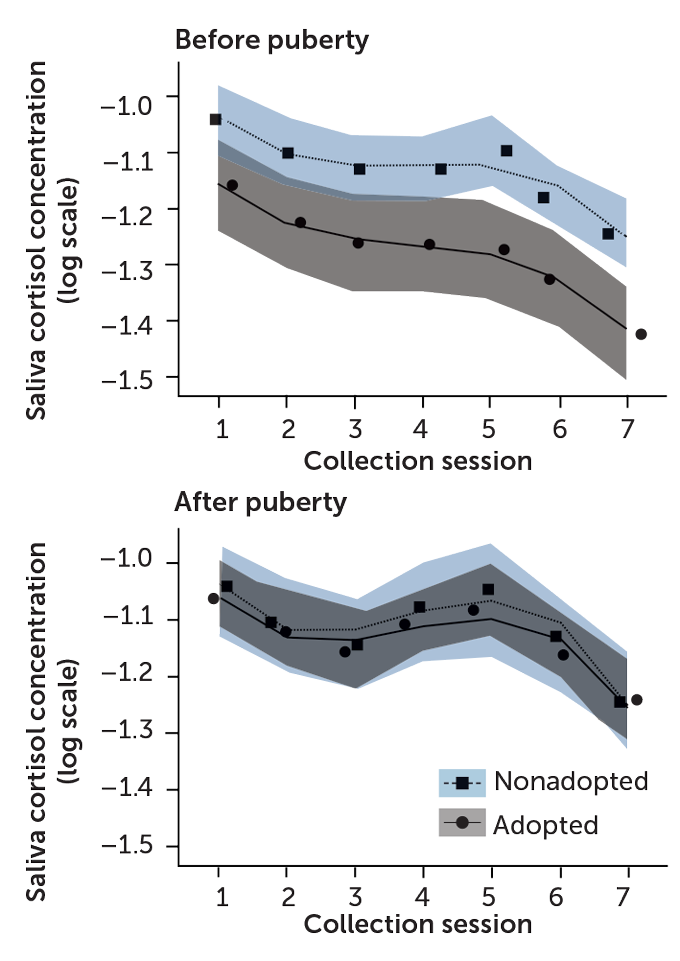
Studying the adoptees over time, she found that preschoolers with low cortisol often entered kindergarten with attention problems. A blunted stress response persisted into middle childhood, even after an average of seven to eight years in a household with healthy caregiving.
That was disheartening, says Russell Romeo, a psychobiologist at Barnard College in New York City. “We’d always thought that maybe if these individuals get out of the adverse situations, they could start recalibrating their stress reactivity.”
But research Romeo had done in the mid-2000s gave Gunnar reason to think she just needed to look further down the road of the children’s lives.
High time for change
Romeo was studying rats to see if stress affects adolescent and adult brains differently. In one set of experiments, he subjected adult rats and prepubescent rats to acute stress — 30 minutes trapped inside a wire mesh container — and recorded their levels of corticosterone (the rat version of cortisol) before, during and after the confinement. Both groups produced similar hormone spikes when stressed, but in the juvenile rats, levels took much longer to return to normal.
When Romeo observed how the animals reacted to extended periods of stress — 30 minutes of restraint each day for seven days — the pattern was different. After the animals were released from the restraints, stress hormones surged higher in young rats than in adults. But the rats that were near puberty returned to baseline more quickly than the older animals. Taken together, Romeo’s studies suggested that neuroendocrine stress responses get shaped during puberty to emerge differently in adulthood.
In earlier work, researchers at McGill University in Montreal showed that moving adolescent rats into “enriched” environments — larger cages with more toys and cagemates — could reset stress responses that had been thrown out of whack by early-life trauma.
These findings heartened Gunnar. “Maybe I should be looking at puberty,” she thought. It could be a time to recalibrate.
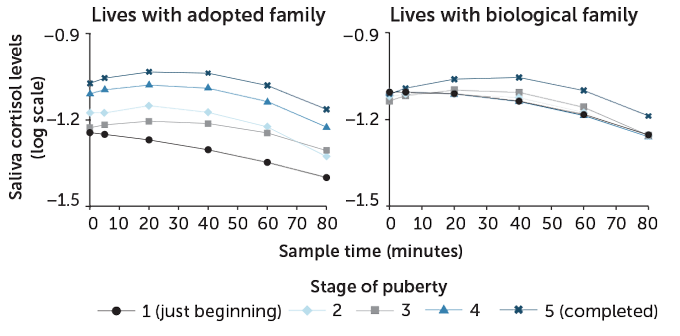
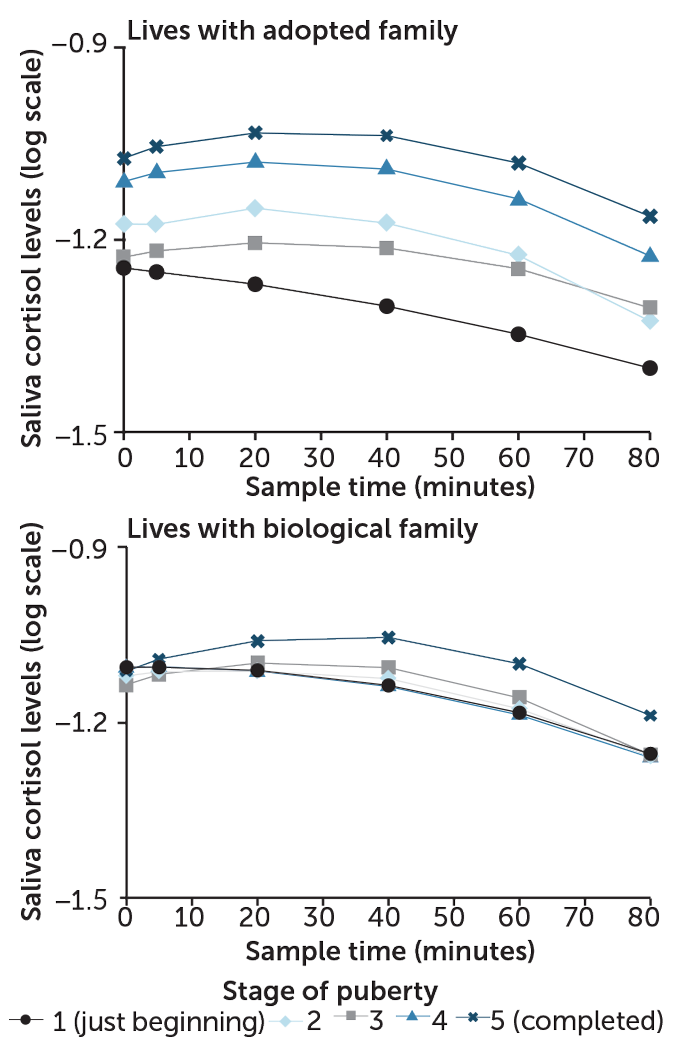
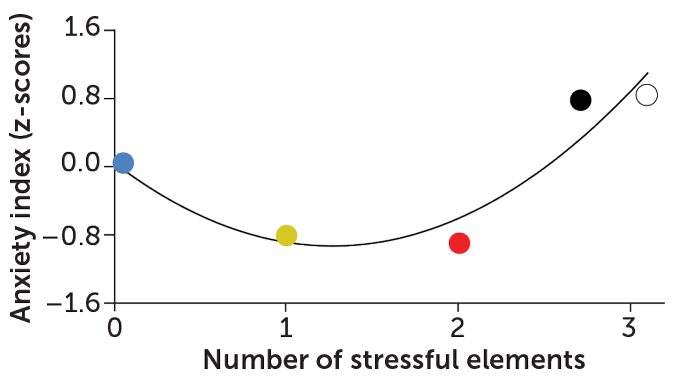
So her team invited 280 7- to 14-year-olds — 122 children adopted from institutions and 158 from socioeconomically comparable biological families — into the lab to complete two stressful tasks. One involved challenging mental math. For the second task, each child prepared a five-minute speech introducing themselves to a new class of students. The children were told that their speech, given in front of a video camera and a mirror, would be rated by judges. Some kids spoke with confidence, while others looked nervous. “We did have one who burst into tears,” Gunnar says. But “we don’t torture them. If we think they’re too nervous, we help them quit.”
Before and after the speech and math tasks, researchers collected saliva samples from each child to measure cortisol levels. Participants’ pubertal status was assessed on a 1-to-5 scale: Stage 1 meant no noticeable body changes and stage 5 meant sexual maturation was complete.
Among kids in early puberty (stages 1–2), adopted kids had blunted cortisol levels before and after the tasks compared with children who lived with their biological parents. This result confirmed Gunnar’s previous research on preschool-aged international adoptees. In the late puberty group (stages 4–5), cortisol patterns looked similar for adopted and nonadopted kids.
To confirm HPA recalibration had occurred within the same child, rather than just comparing across age groups, Gunnar and colleagues brought participants in for the same tests one and two years later, for a total of three annual sessions.
The results, reported in the Nov. 26 Proceedings of the National Academy of Sciences, show the body can recalibrate its response to stressors during puberty. In other words, something happens in puberty — but not earlier in childhood — that allows the brain to shift back to normal stress responses that had been skewed by early trauma.
Matthew Duggan, a therapist in Long Beach, Calif., who specializes in childhood and adolescence, is encouraged by the findings and thinks they could apply to a wide range of children who have trouble managing their emotions and connecting with others because caretakers abused or ignored them early in life. There may be “a window … where things might be able to change,” Duggan says. “And we have some data here to suggest that at a biological level, that is a possibility. For me, that’s really hopeful to see.”
Duggan says Gunnar’s study would have been even more useful if it had assessed participants’ behavior change — for example, by interviewing parents, teachers or the adolescents themselves.
How might puberty combine with better caregiving and support to reshape neuroendocrine stress responses? Romeo speculates that it stems from the fact that the hypothalamus and other brain areas, such as the prefrontal cortex, that control our reactions to stress are among the regions that rewire and strengthen connections during adolescence.
Whether those changes in the stress response will ultimately harm or help a young person is hard to predict, Gunnar says. Mental health and resilience emerge from an ever-changing combination of genes and life experiences — some of which set the body awry early on. But adolescence could potentially erase some of the damage, her research shows. Gunnar and others hope to reveal more of the underlying biology behind the reboot.