This post was originally published on this site
When Nigerian physician Garba Iliyasu was 10, a venomous snake bit a family member. The man survived, but “it was quite severe,” Iliyasu recalls. “[He] was bleeding profusely.… From the nose. From the mouth. From the ear.”
Since then, Iliyasu, a specialist in infectious and tropical diseases, has tended to hundreds of snakebite victims at Kaltungo General Hospital, a health care hub for the surrounding Gombe State. During the two annual peaks in snakebite cases — the spring planting and autumn harvest seasons — “we see like six, seven to 10 patients in a day, on average,” he says. The hospital has only a few dozen beds. “Most times, you see patients on the floor.”
In the Western world, snakebites are a minor issue. In the United States and Europe, cases are rare and hardly ever fatal. Even in Australia — notorious for its deadly, venomous snakes — bites account for just a handful of annual deaths.
But in sub-Saharan Africa, about 270,000 people are bitten every year, resulting in more than 55,000 cases of post-traumatic stress disorder, over 14,700 amputations and about 12,300 deaths, Iliyasu and colleagues estimated in Toxicon in March 2019. Add in India and other snakebite hot spots and the annual numbers rise to more than 2 million bites that need clinical treatment, according to the World Health Organization. Between 80,000 and 138,000 victims die, and about three times that number have a life–changing disability.
Snakebites are “a neglected disease that affects the neglected section of the society,” Iliyasu says. The worst effects occur in mostly poor, rural communities that depend on farming and herding. Visit these places, he says, and “you will see how devastating the effect of snakebite is.” Victims are often the primary breadwinners of their households, so every death and disability contributes to the cycle of poverty.
But snakebites are finally getting the attention they’ve long needed. In 2017, the WHO officially recognized snakebites as a neglected tropical disease. That designation has led to an influx of funding for innovative research; the largest, more than $100 million, came in 2019 from the Wellcome Trust.
Effective snakebite treatments do exist, and those antivenoms are considered the “gold standard” of care. If a victim receives the right antivenom soon after a bite — within an hour or two — then the chances of survival are “very, very high,” says Nicholas Casewell, a biomedical scientist at the Liverpool School of Tropical Medicine in England.
But that “if” looms large, with big challenges remaining, including the difficulties of speedy access to care and the fact that most anti-venoms work against just a few of the hundreds of dangerous species of venomous snakes. Antivenoms are also “a technology that has seen limited innovation for 120 years,” says Andreas Laustsen, a biotech researcher and entrepreneur at the Technical University of Denmark in Kongens Lyngby.
Now, researchers from disparate fields of science are coming together to reimagine the way snakebites are managed. Casewell, Laustsen and others are tweaking current treatments, repurposing pharmaceuticals and even engineering toxin-stopping nanoparticles. The work offers hope that people everywhere, even in remote areas, will eventually be able to safely coexist with snakes.
A tarnished gold standard
There’s a saying in snakebite care that “time is tissue.” The longer it takes to stop a snake’s venom from moving through the victim’s body, the more damage occurs. Destruction begins from the moment of a bite, and the cocktail of proteins and other molecules in the venom will continue to ravage until the immune system produces enough antibodies to remove or destroy those toxins. The problem is, by the time antibodies have ramped up, it’s often too late.
The tissue maxim is especially true for bites from vipers and other snakes with venoms that target the blood and soft tissues and thus tend to cause more physical damage. But speed is also important for bites from snakes with paralytic venoms, such as the Indian cobra (Naja naja) and southern Africa’s black mamba (Dendroaspis polylepi). Their nerve cell–targeting toxins will progressively slow muscles until the lungs and heart stop working.
That’s where antivenoms come in. They speed up the immune system’s clearance of toxins, because antivenoms are, themselves, antibodies pulled from the blood of large animals, usually horses, that have been injected with venom. When given soon after a snakebite, antivenoms work well.
But for myriad reasons, fast delivery often doesn’t happen.
In rural communities, there may be relatively few health care providers who can stock and administer the intravenously delivered drugs, which often require refrigeration. In India, for instance, the staff in rural public health clinics rarely have the resources or training to safely administer the drugs and monitor for treatment side effects.

Patients are often sent several hours away to larger regional hospitals with more expertise. “A lot of [bite victims] die on the way,” says Kartik Sunagar, an evolutionary biologist at the Indian Institute of Science in Bangalore. Sunagar wrote about the challenges of developing antivenoms with Casewell, Laustsen and venom scientist Timothy Jackson of Liverpool in the August Trends in Pharmacological Sciences.
Once a patient arrives at a hospital, delays can still occur, Laustsen says, because medical staff wait until they’re completely sure someone needs antivenom before administering it. A large portion of snakebites are “dry,” which means no venom is injected, so antivenom isn’t always required.
Deciding which antivenom to use can be difficult. To glom on to and remove toxic substances, antibodies need to match their target almost exactly. And since each snake species makes its own unique blend of toxins, most venoms need a specific antivenom. Because bite victims can rarely reliably identify the species that bit them, doctors must wait for clear signs of damage to emerge to determine the right antivenom.
A “better safe than sorry” approach may seem warranted, but injecting antivenom when it’s not needed or if it’s the wrong kind can put the patient at even greater risk. As helpful as horse-derived antibodies can be, “the human immune system will recognize them as foreign,” Laustsen notes, and may launch an attack. This reaction to the antivenom itself can be life-threatening if not treated promptly.

Friendlier options
For the last decade or so, researchers have been working to take horses out of the equation to make antivenoms safer — and maybe more affordable. Laustsen is exploring a couple of approaches to avoiding the body’s reactions to horse-made antibodies.
One option is to produce “humanized” antibodies in the lab by replacing the ends of a human antibody gene with the venom-neutralizing parts from an effective equine antibody gene, so the patient’s body wouldn’t see the antibody proteins as foreign. But, even better, he hopes to discover effective fully human antibodies. With both approaches, he says, “you would remove at least 90 percent of all the side effects.”

Taking horses out of the mix may also open the door for designing antibodies that work against venoms from more than a few species. Laustsen and colleagues described one promising approach July 1 in Scientific Reports. The key is to take human antibody genes and insert them into bacteria-infecting viruses, which build the antibodies into their shells.
Since large databases of human antibody genes already exist, a whole variety of different human antibodies can be inserted into viruses for high-throughput testing to find antibodies that can bind to — and perhaps neutralize — venom toxins.
As a proof of concept, Laustsen’s team tested 40 billion antibodies from people, and identified one particularly exciting candidate: It protected human cells in lab dishes from more than a dozen lethal toxins from three cobra species.
Once the most broadly effective antibodies are found, Laustsen hopes to copy a page from the insulin-production handbook. For diabetes treatment, insulin used to be extracted from the pancreases of animals; now, it’s made by engineered bacteria in large fermentation tanks. A similar process could work to produce broad-spectrum antivenom, he says.
Moving antibody production out of animals could also have another important benefit: lower production costs. Right now, “antivenom is one of the most expensive drugs that you can find in the rural areas,” explains Muhammad Hamza, a medical doctor who, like Iliyasu, splits his time between research at Nigeria’s Aminu Kano Teaching Hospital and treating patients at the regional treatment center in Gombe State. Many of Hamza’s patients could be saved by antivenom, he says, but they can’t afford to pay for it. If the government hasn’t kept the clinic stocked with free medicine, patients die.
In Nigeria, a vial of antivenom costs around $60 to $70, Iliyasu says. He’s seen patients sell their animals, homes and farms to pay for treatment.
Antivenoms engineered without animals would save patients money because the ideal mix of antibodies would be more potent. At least 70 percent of the antibodies in current antivenoms don’t neutralize venom toxins at all, Iliyasu notes. As a result, it often takes several vials of antivenom — sometimes as many as 10 — to treat a bite patient. Boosting the percentage of neutralizing antibodies in each vial would go a long way toward making antivenoms affordable, Iliyasu says — and that’s why he’s excited to see the move away from animal-based production.
A pill for snakebite
Other researchers are turning to existing drugs to expand options for snakebite treatments.
Venom toxins generally cause harm by performing specific molecular actions, such as cutting up certain proteins or fats within cells. Targeted molecules that interfere with that nefarious work could potentially stop the toxins.
The idea of using drugs other than antibodies to inhibit venom toxins isn’t new. But it wasn’t until the molecular and genetic technology revolutions of the late 20th century that scientists could really deconstruct venoms to figure out which components are responsible for a venom’s worst effects. “We now have a very good handle on what the toxins are,” Casewell says.
It’s unlikely that one drug, or even a combination, would be able to neutralize the diversity of harmful toxins present in snake venoms and work as effectively as traditional antivenoms. But Casewell’s aim isn’t to replace antivenoms; he wants to safely slow down the most pernicious venom toxins to buy patients time to get to a clinic.
He and colleagues have so far focused on metalloproteinases — toxins that chop up proteins and are major players in the lethal and destructive nature of tissue-destroying venoms, such as those in saw-scaled vipers (Echis spp.). Casewell’s group picked a few drugs already on the market that bind up the metal ions that these proteinases need to function, and right off the bat, the drugs were surprisingly successful.
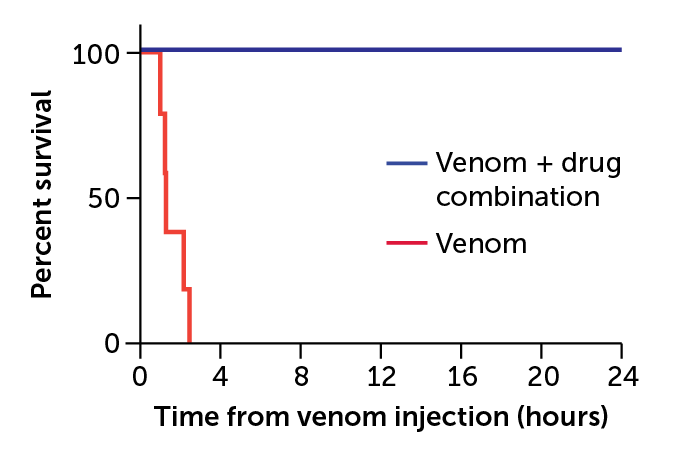
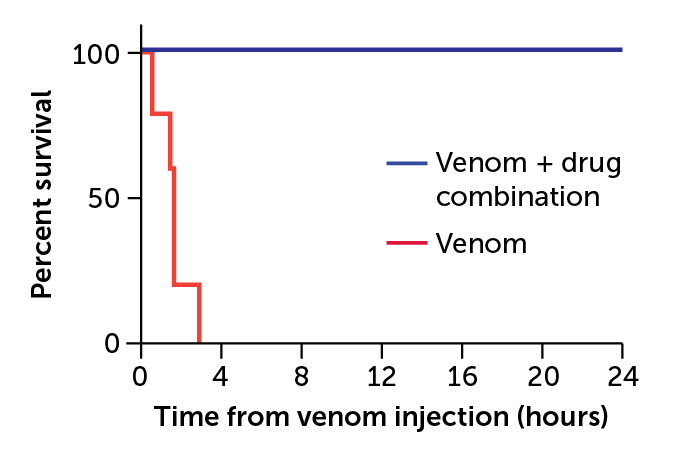
The group demonstrated that an existing small molecule drug used to treat heavy metal poisoning could reduce the deadly damage of viper bites in lab animals (SN: 6/6/20, p. 12). And when paired with another drug that inhibits a family of toxins that chew up certain fats, the drug was even more powerful. In animal tests, the combination neutralized the venoms of a more diverse collection of five snake species from all over the world.
The work is “quite exciting,” Casewell says, because it means small molecule drugs might be able to overcome the problem of geographic fragmentation — each venom needs its own antidote — that keeps antivenom markets too small and nonlucrative for pharmaceutical companies to invest in.
As a bonus, such small molecules are available in pill form and don’t need refrigeration or expert administration, making them easier to distribute in rural communities. In that way, such drugs could become an important “bridge to care,” Iliyasu says.
Next generation of treatments
While pills alone may never be a stand-alone treatment for snakebites, there are other alternatives to conventional antivenoms, says Shih-Hui Lee of the University of California, Irvine. “We can use a polymer.”
Lee and colleague Kenneth Shea are new to the field of snakebite treatment. “We’re not snake venom people,” Shea admits. They’re not even biologists. The two are materials scientists. But their approach to overhauling antivenom is so out of the box that it’s getting noticed.
Both spent much of their careers designing carbon polymers — essentially, plastic nanoparticles — with specific, desirable properties. After a while, the duo started to wonder if their designer plastics, which could bind to certain parts of proteins, could mimic the actions of antibodies.
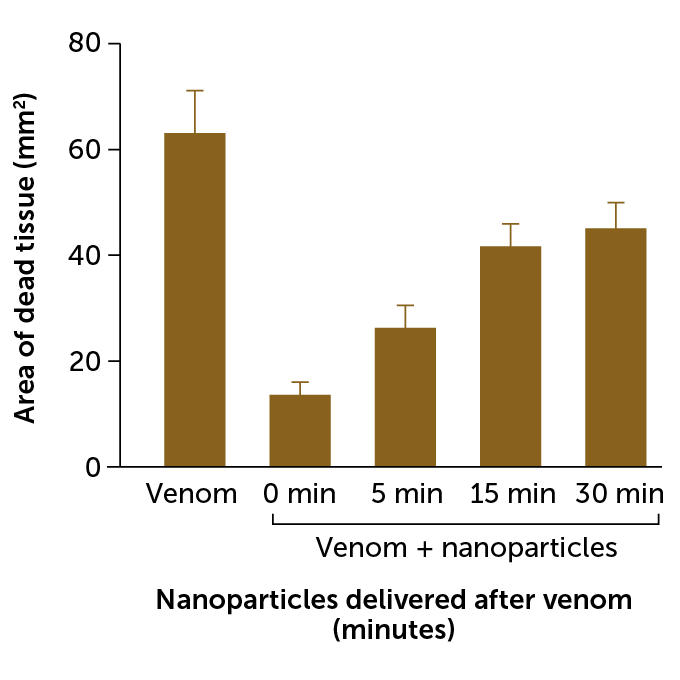
Shea started with melittin, a bee venom toxin. To his surprise, the polymer nanoparticles worked. When injected into mice shortly after the injection of a life-threatening dose of melittin, the particles bound up enough of the toxin to save the animals’ lives, Shea and colleagues reported in the Journal of the American Chemical Society in 2010.
Those results helped him recruit Lee to the antivenom project and convince well-respected snakebite expert José María Gutiérrez of the University of Costa Rica in San José to collaborate. With his help, Shea and Lee set their sights on phospholipase A2s, a large family of toxins found in many deadly snake venoms.
Once again, Lee says, the polymer nanoparticles neutralized the toxins. In 2018, the particles proved effective against another family of snake toxins called three-finger toxins. The “plastic” antibodies saved mice from cobra venom, and healthy mice that received them had no adverse reactions, the team reported in PLOS Neglected Tropical Diseases.
There are still some design challenges to overcome before testing the polymers in people. The team wants to put these synthetic antibodies into injectable devices — much like an EpiPen — but right now, the nanoparticles are probably too big. So the next hurdle is to make them smaller and more able to travel from the injection site in a muscle to the surrounding tissues.
But the biggest challenge is convincing funding agencies that synthetic antibodies should be on the table. The hesitancy is understandable, Shea says, as there’s nothing like these nanoparticles on the market. “This is untested, so there has to be an element of faith in this,” he says.
Still, Shea and Lee believe in their creation. Producing a broad-spectrum antivenom with the nanoparticles “is technically much less challenging” than with biological antibodies, Shea says, so if the team can secure investors, he thinks the nanoparticles have the potential to be “a quite cheap antidote.”
Others are stepping out of the box, as well. Thanks to the influx of funding in the last few years, researchers around the world are trying all sorts of unconventional approaches to snakebite remedies. There are labs hoping to design DNA molecules known as aptamers that act like antibodies. Others are turning to animals, such as opossums, that are naturally immune to venoms in the hopes of translating that immunity into new drugs. All of this work is leading to some truly exciting technological developments, Casewell says.
But none of it will matter if there aren’t also investments in infrastructure and education, Hamza warns. “It is one thing to have the drug.… It’s another thing to get it available to the remotest parts of the world.”
He’s more excited about smartphone apps that could tell people in remote areas where the closest available antivenom is, for instance. And something as simple as providing farmers solid boots with instructions on when and why to wear them could prevent countless snakebites from happening in the first place.
With millions of snakebites occurring every year, there’s certainly many opportunities to improve the situation — and all of them need attention, Casewell says. That attention is finally coming. “This is kind of a once-in-a-lifetime moment for snakebites,” he says.