SACRAMENTO — A judge has initiated a federal court takeover of California’s troubled prison mental health system by naming the former head of the Federal Bureau of Prisons to serve as receiver, giving her four months to craft a plan to provide adequate care for tens of thousands of prisoners with serious mental illness.
Senior U.S. District Judge Kimberly Mueller issued her order March 19, identifying Colette Peters as the nominated receiver. Peters, who was Oregon’s first female corrections director and known as a reformer, ran the scandal-plagued federal prison system for 30 months until President Donald Trump took office in January. During her tenure, she closed a women’s prison in Dublin, east of Oakland, that had become known as the “rape club.”
Michael Bien, who represents prisoners with mental illness in the long-running prison lawsuit, said Peters is a good choice. Bien said Peters’ time in Oregon and Washington, D.C., showed that she “kind of buys into the fact that there are things we can do better in the American system.”
“We took strong objection to many things that happened under her tenure at the BOP, but I do think that this is a different job and she’s capable of doing it,” said Bien, whose firm also represents women who were housed at the shuttered federal women’s prison.
California corrections officials called Peters “highly qualified” in a statement, while Gov. Gavin Newsom’s office did not immediately comment. Mueller gave the parties until March 28 to show cause why Peters should not be appointed.
Peters is not talking to the media at this time, Bien said. The judge said Peters is to be paid $400,000 a year, prorated for the four-month period.
About 34,000 people incarcerated in California prisons have been diagnosed with serious mental illnesses, representing more than a third of California’s prison population, who face harm because of the state’s noncompliance, Mueller said.
Appointing a receiver is a rare step taken when federal judges feel they have exhausted other options. A receiver took control of Alabama’s correctional system in 1976, and they have otherwise been used to govern prisons and jails only about a dozen times, mostly to combat poor conditions caused by overcrowding. Attorneys representing inmates in Arizona have asked a judge to take over prison health care there.
Mueller’s appointment of a receiver comes nearly 20 years after a different federal judge seized control of California’s prison medical system and installed a receiver, currently J. Clark Kelso, with broad powers to hire, fire, and spend the state’s money.
California officials initially said in August that they would not oppose a receivership for the mental health program provided that the receiver was also Kelso, saying then that federal control “has successfully transformed medical care” in California prisons. But Kelso withdrew from consideration in September, as did two subsequent candidates. Kelso said he could not act “zealously and with fidelity as receiver in both cases.”
Both cases have been running for so long that they are now overseen by a second generation of judges. The original federal judges, in a legal battle that reached the U.S. Supreme Court, more than a decade ago forced California to significantly reduce prison crowding in a bid to improve medical and mental health care for incarcerated people.
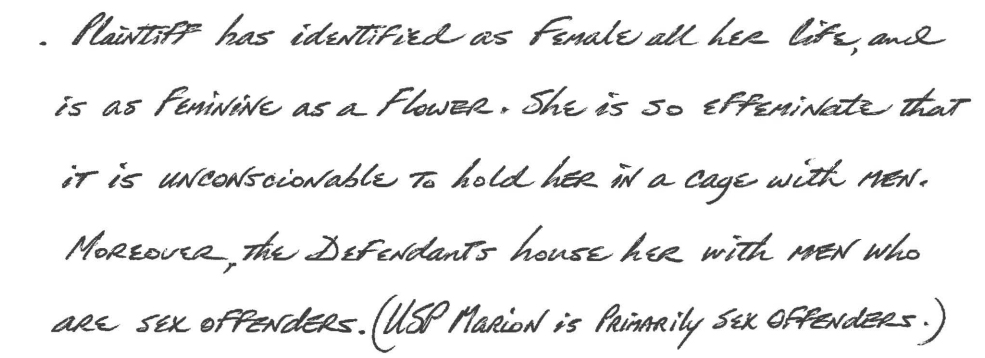
State officials in court filings defended their improvements over the decades. Prisoners’ attorneys countered that treatment remains poor, as evidenced in part by the system’s record-high suicide rate, topping 31 suicides per 100,000 prisoners, nearly double that in federal prisons.
“More than a quarter of the 30 class-members who died by suicide in 2023 received inadequate care because of understaffing,” prisoners’ attorneys wrote in January, citing the prison system’s own analysis. One prisoner did not receive mental health appointments for seven months “before he hanged himself with a bedsheet.”
They argued that the November passage of a ballot measure increasing criminal penalties for some drug and theft crimes is likely to increase the prison population and worsen staffing shortages.
California officials argued in January that Mueller isn’t legally justified in appointing a receiver because “progress has been slow at times but it has not stalled.”
Mueller has countered that she had no choice but to appoint an outside professional to run the prisons’ mental health program, given officials’ intransigence even after she held top officials in contempt of court and levied fines topping $110 million in June. Those extreme actions, she said, only triggered more delays.
The 9th U.S. Circuit Court of Appeals on March 19 upheld Mueller’s contempt ruling but said she didn’t sufficiently justify calculating the fines by doubling the state’s monthly salary savings from understaffing prisons. It upheld the fines to the extent that they reflect the state’s actual salary savings but sent the case back to Mueller to justify any higher penalty.
Mueller had been set to begin additional civil contempt proceedings against state officials for their failure to meet two other court requirements: adequately staffing the prison system’s psychiatric inpatient program and improving suicide prevention measures. Those could bring additional fines topping tens of millions of dollars.
But she said her initial contempt order has not had the intended effect of compelling compliance. Mueller wrote as far back as July that additional contempt rulings would also be likely to be ineffective as state officials continued to appeal and seek delays, leading “to even more unending litigation, litigation, litigation.”
She went on to foreshadow her latest order naming a receiver in a preliminary order: “There is one step the court has taken great pains to avoid. But at this point,” Mueller wrote, “the court concludes the only way to achieve full compliance in this action is for the court to appoint its own receiver.”