This post was originally published on this site
When I talk to immunologist Paul Morgan, he’s on the hunt for potentially life-altering drugs.
He’s got a call with a pharmaceutical company planned in the next half hour. His goal: persuade the company to supply his lab with a drug that might — maybe, hopefully, someday — ease some of the unrelenting symptoms of long COVID.
Morgan’s lab at Cardiff University in Wales has been studying people with the disease, including the first waves of patients, some of whom have been living with long COVID for more than two years (SN: 8/21/23). The “very long haulers,” he calls them. Their symptoms can include brain fog, fatigue, breathlessness and joint and muscle pain.
Morgan and his colleagues have pinpointed an immune system anomaly in the blood of some of these long haulers. A drug that targets that quirk might be one way to treat their disease. He’s quick to tell me that this research is in its early days. First, his team needs to get its hands on a drug. Then they need to do a clinical trial — at this stage, it’s still proof-of-concept. “Actual treatments are still some way off,” he says.
But the work is one in a surge of studies mining the blood for long COVID clues, potential biomarkers of the disease. A growing cadre of labs are starting to sketch out some of the shrouded figures at play in the once-seemingly inscrutable disease. It’s as if there’s a “picture that’s being revealed from the fog,” says Akiko Iwasaki, an immunologist and Howard Hughes Medical Institute investigator at Yale University.
That picture features a motley cast of molecular and cellular characters that could point scientists toward potential tests and treatments — both are currently lacking. Still, the full long COVID landscape is unquestionably complicated. Assorted actors tangle together in an immunological thicket that can make the disease seem impenetrable.
But Iwasaki thinks researchers can crack long COVID’s mysteries. In fact, recent work in the field has her feeling pretty excited. Yes, investigating long COVID is complex, she says. “But it’s definitely worth doing because many people are suffering.”
I spoke with Iwasaki, Morgan, and other researchers about long haulers and current work to illuminate the disease — and to get clarity on the less severe but still vexing symptoms that stuck around for months after my own COVID-19 infection.
Long COVID is not a single disease, which makes diagnosis and treatment difficult
Some 5 to 20 percent of COVID-19 cases develop into long COVID, though the exact number is hard to pin down. One formidable challenge is diagnosis. Does a person with bone-deep exhaustion and trouble concentrating on the pages of their book have the disease? There’s no test or nasal swab doctors can use to provide a definitive answer.
For diseases like diabetes and prostate cancer, scientists look for biomarkers in the blood — molecules that can serve as telltale signs of illness. But “we are not likely to come up with one biomarker or even one set of biomarkers to distinguish everyone with long COVID,” Iwasaki says.
The difficulty is that long COVID is not just one disease. It’s likely a collection of many diseases, she says, with varying sets of symptoms and triggers. Even defining long COVID is complicated. Last spring, researchers developed a long COVID scoring system that factors in a dozen signature symptoms. But more than 200 symptoms have been tied to the disease, and cases can vary greatly from person to person (SN: 11/17/22).
Today, in many doctors’ offices and clinics, homing in on a diagnosis means first ruling out other conditions. For example, after months of feeling wrung out and faded, with unexpected pain in my legs following a COVID-19 infection last year, my doctor ordered a slew of blood tests. She was looking for signs of rheumatoid arthritis, Lyme disease, thyroid hormone abnormalities and a handful of other conditions. Everything was negative. It’s called a “diagnosis of exclusion,” Morgan says. “You test for everything else, and when nothing comes back positive, you say, ‘well, it must be [long COVID], then.’”
He compares it to myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS, another debilitating condition that also lacks clear diagnostic tests. “Many physicians don’t take it very seriously at all because of that.” That concern is even listed on the U.S. Centers for Disease Control and Prevention’s ME/CFS Web page. And it’s true of long COVID, too, says Wolfram Ruf, an immunologist at University Medical Center Mainz in Germany. “There’s still some misconception that this is just a psychological disease.” A 2022 survey found that a third of long COVID patients felt as if medical professionals dismissed their illness. And stories from frustrated long haulers continue to appear in the news.
Better diagnostics mean people suffering from long COVID’s myriad symptoms could put a firm label on their condition. That’s important, Morgan says. But tests that spot long COVID biomarkers in the blood could also do far more. “If those tests actually lead you to a mechanism and to a treatment,” he says, “then that’s transformational.”
A complicated cast of immune and other characters may contribute to long COVID
Morgan’s lab and others have zeroed in on immune proteins that defend us from bacteria and viruses. These proteins, part of a defense called complement, circulate in the blood, and get chopped up during an infection. The resulting fragments sound a “we’re under attack” alarm and help form a molecular machine that busts pathogens.
Once the infection clears, the fragments fade away. But in some people with long COVID, the alarm-raising fragments can linger in the blood, Morgan’s team reported February 14 in Med. That’s a sign that the defense system is still whipping up inflammation — in some cases, even years after a person’s initial COVID-19 infection. In January, a different group reported something similar in Science in a study of 113 COVID-19 patients.
Not everyone with long COVID will have complement abnormalities. Even in the patients Morgan studies, “there will be some people who have no changes in their complement markers at all.”
But for those who do, it can be a double-edged sword, he says. Turning complement on briefly can knock out some bugs, but keeping it on chronically can damage your cells.
There’s an ever-growing list of other blood-borne anomalies, too. A protein found in the brain can leak out into the blood in people with brain fog, scientists found in February. And long COVID patients can have low levels of the stress hormone cortisol, Iwasaki’s team reported in Nature in September. In some patients, she and others have also spotted other suspicious signs, like long-slumbering herpes viruses that reawaken and start infecting cells again. “Whether this is a cause or effect [of long COVID],” Iwasaki says, “we don’t know.” Usually, the immune system keeps these viruses under control.
In some people with long COVID, powerful immune players called T cells also seem to go out of whack. Scientists in England analyzing the blood of long COVID patients found T cells that release high levels of an alarm signal called interferon-gamma. That signal could serve as a potential biomarker in some patients, the study’s authors suggested.
“Perhaps there’s SARS-CoV-2 somewhere in the body that can’t be cleared.”
Nadia Roan
At the University of California, San Francisco, virologist and immunologist Nadia Roan’s team is also taking a look at T cells. In some long COVID patients, T cells that recognize SARS-CoV-2 can become exhausted, her team reported in Nature Immunology in January. And scientists know that tired-out T cells can have trouble wiping out infection.
“Perhaps there’s SARS-CoV-2 somewhere in the body that can’t be cleared,” Roan says. If a hidden reservoir of virus lurks in people’s tissues long-term, certain T cells might gather there for continued attack, eventually wearing the cells down. Last summer, a different team found viral traces in some people’s guts nearly two years after their initial infection. Scientists have also spotted signs of SARS-CoV-2 in other body tissues, including brain, lung and liver. These traces may be enough to irritate the immune system long term.
Residual virus isn’t likely to explain everything. “Different mechanisms may drive different forms of the disease,” Roan says. But together, work from her lab and others paints a portrait of an immune system under enduring duress. And as the pictures comes into focus, scientists are starting to explore new experiments, trials and treatments.
Clinical trials will test whether antiviral drugs can ease long COVID symptoms
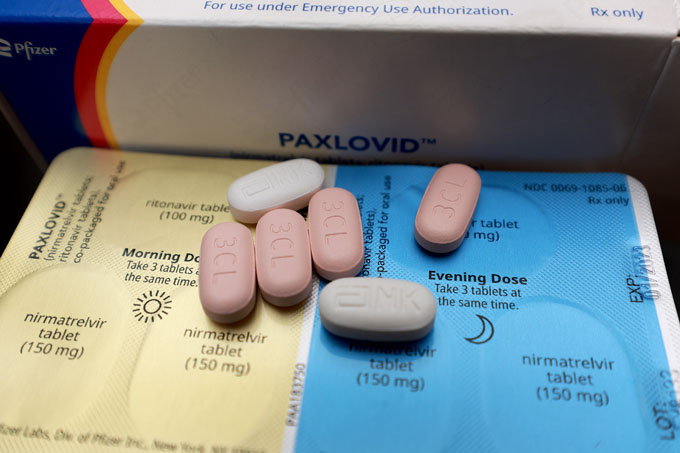
Iwasaki and her colleagues are nearly done recruiting 100 people with long COVID for a randomized clinical trial of the antiviral drug Paxlovid. A similar trial by the National Institutes of Health is also in the works. That study aims to enroll 900 people and should conclude testing by this summer.
An idea targeted by both trials is that SARS-CoV-2 persists in the body, triggering symptoms. Scientists will follow participants as they take Paxlovid for 15 or 25 days. (For COVID-19 infection, the typical treatment length is five days.)

Iwasaki’s team also plans to scan participants’ blood for molecules that might predict a person’s response to Paxlovid. Suppose participants who improve after Paxlovid had high levels of certain blood molecules prior to treatment. Scientists could then measure those molecules in other people with long COVID to see if they might be good candidates for the drug. “There’s not one drug cure-all,” Iwasaki says, “but even knowing who might benefit is a huge thing.”
And though Morgan’s complement work is still at an early stage, he considers it a “strong lead to a potential therapy.” One bright spot is the number of complement-targeting drugs that already exist. Doctors currently use the drugs to treat certain blood disorders and other rare conditions. Morgan and other scientists have tried using some of these drugs to treat severe cases of acute COVID-19 infection, but large-scale trials didn’t pan out.
Now, he wants to repurpose those drugs for long COVID patients whose complement system has gone out of control. Dialing down those defenses might help quench the fire of chronic inflammation.
So far, Morgan hasn’t seen much interest from pharmaceutical companies. Repurposing generic drugs isn’t a big money maker. And Morgan’s team doesn’t envision long COVID patients needing to use the drugs long-term — another financial disincentive for companies. But when I email him later, he says his call after our interview went well. Morgan’s not naming the company yet but he knows that patients are standing by, waiting day after day for anything that will offer some relief.
For me, lingering symptoms turned the once-easy tasks of everyday life into energy-sucking feats performed while my body’s battery blinked down to zero. If I miscalculated and walked too fast or moved too much, I’d pay for it later and crash on the couch or in bed, sometimes taking days to recover. That symptom is known as post-exertional malaise and it’s common for people with long COVID.
But I was never officially diagnosed with the disease. Keeping up with doctors’ appointments felt daunting, and I wasn’t sure how much my doctor would be able to help. There may be many people who fall into this category, Morgan says — people who have long-term symptoms but lack clear-cut answers.
Though white women like myself are most likely to be diagnosed with the disease, in a survey from the U.S. Census Bureau, Hispanic and Black people were more likely to report long-lasting symptoms. Access to care could be one factor in the diagnosis discrepancy. Previous data have shown that people from these groups are less likely to have health insurance. Another factor may be the changeling nature of the disease itself. Long COVID can show up differently in different groups of people, scientists have found.
I’m lucky because my symptoms started improving after about six months. I knew I was mostly recovered the first time I went grocery shopping and carried my bags into the house by myself, without crashing afterwards. But so many others continue to struggle.
Morgan sees that firsthand. Since his paper came out, “I’ve been absolutely deluged by letters from patients,” he says. They ask to be tested and if he has drugs that can treat them. For Morgan, those letters show the depth of the problem.
“I reply to them all,” he says.