The drug buprenorphine is an effective treatment for opioid use disorder, but many who misuse opioids also take benzodiazepines — drugs that treat anxiety and similar conditions. Many treatment centers hesitate to treat patients addicted to opioids who also take benzodiazepines. Researchers at Washington University School of Medicine in St. Louis studied overdose risk in people taking buprenorphine and found that the drug lowered risk, even in people taking benzodiazepines.
Tag: user_id 13800
FAIR Health releases study on impact of COVID-19 on pediatric mental health
In March and April 2020, mental health claim lines for individuals aged 13-18, as a percentage of all medical claim lines, approximately doubled over the same months in the previous year.
Financial Incentives for Hospitals Boost Rapid Changes to Opioid Use Disorder Treatment
In a study at Penn researchers found that Pennsylvania’s financial incentive policy encouraged hospitals to enact rapid changes to support treatment for opioid use disorder for patients visiting the ED, and evaluates the efficacy of the Opioid Hospital Quality Improvement Program.
UNH Receives Nearly $3 Million to Research Effectiveness of Wilderness Therapy
The University of New Hampshire’s Outdoor Behavioral Healthcare Center will receive $2.97 million in grants to conduct a first-of-its-kind randomized study looking at the effectiveness of outdoor behavioral health (OBH), or wilderness therapy, a prescriptive treatment for teens struggling with depression, anxiety and substance use disorders.
Cigna Designates Henry Ford Maplegrove as a Center of Excellence for Substance Use Treatment
WEST BLOOMFIELD, MI (February 23, 2021)–Henry Ford Maplegrove Center is pleased to announce that it has been designated as a Cigna Center of Excellence for Substance Use. The designation recognizes top performing addiction recovery centers that provide patients with quality care, an exceptional experience and cost efficiency.
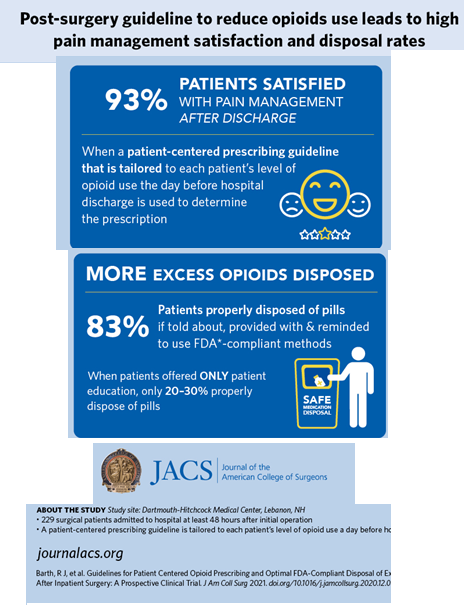
Guideline for reducing opioid use post-surgery leads to high pain management satisfaction and disposal rates
A prescribing guideline tailored to patients’ specific needs reduced the number of opioid pills prescribed after major surgery with researchers reporting a greater than 90 percent patient satisfaction rate with pain management and the highest compliance rate to date with appropriate disposal of leftover pills. The study was selected for the 2020 New England Surgical Society Program and published as an “article in press” on the website of the Journal of the American College of Surgeons (JACS) in advance of print.
The researchers focused on a post-surgery opioid prescribing guideline developed by surgeons at the Dartmouth-Hitchcock Medical Center, Lebanon, N.H. The guideline is based on the number of opioids patients take on the day before they are discharged from the hospital.
Lead study author Richard J. Barth Jr., MD, FACS, section chief of general surgery, explained that the guideline recommends discharging patients with no prescription for opioids if they have taken no opioids on the day before; 15 pills if they have taken one to three pills; and 30 pills if they have had four or more pills.
“This guideline was designed to satisfy the pain management needs of about 85 percent of patients,” said Dr. Barth, who led a previous study published in JACS in 20181
that proposed the guideline and showed that the number of opioids taken the day before discharge was the best predictor of how many opioids patients used after discharge.
The 2018 study involved only general surgery procedures, whereas the latest study included a broader cross-section of surgery: general surgery, as well as colorectal, gynecological, thoracic, and urological operations.
“In this new prospective study we found that 93 percent of patients had their post-surgery opioid needs satisfied,” Dr. Barth said of the most recent JACS study.
“This finding means that this guideline can be used for a wide variety of operations to guide surgeons on how many opioids to prescribe when sending patients home after surgery.”
Researchers consider patient’s perception of pain
This study is unique because it’s a prospective one of a post-surgery pain management guideline that takes into account an individual patient’s perception of pain. A prospective study enrolls patients before they’ve achieved the study outcome—in this case, an operation and their opioid use afterward—whereas a retrospective study evaluates outcomes after the fact. Other guidelines, which base the number of opioids prescribed solely on the operation that was performed, do not take into account individual variations in patients’ responses to pain. Minimizing opioid use among surgical patients is an important strategy for medicine because studies have found that up to 10 percent of patients who have undergone surgery, but have not used opioids before, may go on to become chronic opioid users.2
Study details
The study enrolled 229 patients admitted to the hospital for at least 48 hours after their initial operation. Upon discharge, patients received prescriptions for the non-opioid medications acetaminophen and ibuprofen, as well as opioids based on the guideline. Researchers used a protocol that deviated slightly from the post-discharge opioid prescribing guideline:
Patients who used no opioids—calculated as zero oral morphine milligram equivalents (MME)—on the day before discharge were sent home with five oxycodone 5-mg pill equivalents (PEs)
Patients who used up to 30 MME received 15 PEs
Patients who used 30 MME or more received 30 PEs
The lower the opioid usage was before hospital discharge, the higher the level of patient satisfaction with pain management: 99 percent of those in the zero-MME group reported satisfaction, as did 90 percent in the middle MME group, whereas 82 percent in the 30-plus MME group did so (P=0.001).
Despite being given an opioid prescription, 73 percent of the zero-MME group used no opioids at home, and 85 percent used two pills or less.
Surgeon’s role in minimizing opioid use
Dr. Barth noted that surgeons play a pivotal role in minimizing opioid use in their patients by setting expectations for pain management. That discussion involves letting patients know they are likely to be discharged with either no opioids or a small amount based on their opioid use on the day before they go home. “Explain to the patient, ‘We’ve studied this issue; we’ve figured out how many opioids you are likely to need,’” he said.
“The other part of that discussion involves letting patients know that they should expect some pain, that our goal isn’t to get rid of every last bit of their pain,” he added. “That was something that surgeons tried to accomplish years ago, but that’s not what we’re aiming for now. A low level of discomfort is acceptable, and patients need to have that expectation.”
That process also involves prescribing, not just recommending, over-the-counter non-opioid analgesics. “By prescribing non-opioid analgesics the surgeon sets the expectation that they should be used,” he said. “It’s a big difference if a surgeon prescribes non-opioid analgesics compared with just recommending that a patient take acetaminophen or ibuprofen that they might have at home.”
He added, “In this study, 95 percent of the patients took either acetaminophen or ibuprofen and 70 percent took both, whereas in previous studies1 where we had just recommended that they use them, 85 percent reported taking one or the other, but only 20 percent reported taking both.”
Opioid disposal rate soars with surgeons’ input
Proper disposal of unused pills is another key component of responsible opioid management. In this study, 60 percent of patients had leftover pills. “We worry about unused pills because those pills could be used by that individual patient and might predispose them for long-term or chronic use,” Dr. Barth said. “Those excess pills could also be diverted to others and perpetuate opioid misuse in the community.”
The Dartmouth-Hitchcock investigators employed several strategies to encourage patients to properly dispose of leftover pills. In addition to educating patients about the potential for opioid misuse and diversion, one strategy was to install a drop box for leftover pills in the institution’s pharmacy, located near the surgeons’ outpatient offices. A phone call before the post-surgery follow-up appointment also reminded patients to bring their unused pills with them to dispose. “These are easily actionable items that can really impact the disposal of excess opioids,” Dr. Barth added.
When these strategies were employed, 83 percent of patients disposed of their excess opioids using a method that complies with Food and Drug Administration recommendations. This rate is substantially higher than rates of disposal in the 20-to-30 percent range reported by other investigators who relied on patient education alone.3 Fifty-one percent of the patients who disposed of their excess opioids used the drop box in the hospital pharmacy, while 28 percent used a drop box in a police or fire department and 21 percent used other FDA-compliant methods of disposal. A total of 2,604 pills were prescribed in the study; only 187 of them (7 percent) were kept by patients.
Three Longtime Antibiotics Could Offer Alternative to Addictive Opioid Pain Relievers
DALLAS – Feb. 22, 2021 – Three decades-old antibiotics administered together can block a type of pain triggered by nerve damage in an animal model, UT Southwestern researchers report. The finding, published online today in PNAS, could offer an alternative to opioid-based painkillers, addictive prescription medications that are responsible for an epidemic of abuse in the U.S.
IU study finds unintended consequences of state, opioid policies
IU study finds unintended and negative consequences of policies designed to reduce the supply of opioids in the population for overdose.
Study finds unintended consequences of state, opioid policies
n response to the increase in opioid overdose deaths in the United States, many states have implemented supply-controlling and harm-reduction policy measures aimed at reducing those deaths. But a recent study from Indiana University found the policies may have had the unintended consequence of motivating those with opioid use disorders to switch to alternative illicit substances, leading to higher overdose mortality.
“Literature from public health to social sciences has presented mixed and contradictory findings on the impact of opioid policies on various opioid adverse outcomes,” said Byungkyu Lee, assistant professor of sociology at IU and co-author of the study. “Our findings suggest that the so-called opioid paradox — the rise of opioid-related deaths despite declines in opioid prescriptions — may arise from the success, not the failure, of state interventions to control opioid prescriptions.”
Researchers used the National Vital Statics System and Optum Clinformatics DataMart to look at drug overdose mortality data from 50 states and claims data from 23 million commercially insured patients in the U.S. between 2007 and 2018. They then evaluated the prevalence of indicators of prescription opioid abuse, opioid use disorder and overdose diagnosis, and the prescription of medications-assisted treatment and drug overdose deaths before and after implementation of six state-level policies targeting the opioid epidemic.
Policies included prescription drug monitoring program access, mandatory prescription drug monitoring programs, pain clinic laws, prescription limit laws, naloxone access laws and Good Samaritan laws.
The study, published in the JAMA Network Open, found that supply-controlling policies were associated a lower proportion of patients who take opioids, have overlapping claims, receive higher opioid doses and visit multiple providers and pharmacies. They also found that harm-reduction policies were associated with modest increases in the proportion of patients with overdose and opioid use disorder. Additionally, the proportion of patients receiving medications-assisted treatment drugs increased following the implementation of supply-controlling policies.
Brea Perry, professor of sociology at IU and co-author of the study, said these findings demonstrate the power of big data to provide insights into the opioid epidemic and how to best reverse it.
“Our work reveals the unintended and negative consequences of policies designed to reduce the supply of opioids in the population for overdose,” Perry said. “We believe that policy goals should be shifted from easy solutions such as dose reduction to more difficult fundamental ones, focusing on improving social conditions that create demand for opioids and other illicit drugs.”
In terms of overdose mortality, the study found that all overdose deaths increased following the implementation of naloxone access laws, especially deaths attributable to heroin, synthetic opioids and cocaine. Good Samaritan laws were also associated with increases in overall overdose deaths.
Furthermore, mandatory prescription drug monitoring programs were associated with a reduction in overdose deaths from natural opioids and methadone, and the implementation of pain clinic laws was associated with an increase in the number of overdose deaths from heroin and cocaine. However, having a prescription limit law was associated with a decrease in overdose deaths from synthetic opioids.
“Our work demonstrates that there is no easy policy solution to reverse the epidemic of opioid dependence and mortality in the U.S.,” Lee said. “To resolve the opioid paradox, it is imperative to design policies to address the fundamental causes of overdose deaths, such as lack of economic opportunity, persistent physical, and mental pain, and enhance treatment for drug dependence and overdose rather than focusing on opioid analgesic agents as the cause of harm.”
Other co-authors of the study are Wanying Zhao, Kai-Cheng Yang and YY Ahn, all from the IU Luddy School of Informatics. This work was supported by a National Institute on Drug Abuse grant.
IU Research
Indiana University’s world-class researchers have driven innovation and creative initiatives that matter for 200 years. From curing testicular cancer to collaborating with NASA to search for life on Mars, IU has earned its reputation as a world-class research institution. Supported by $854 million last year from our partners, IU researchers are building collaborations and uncovering new solutions that improve lives in Indiana and around the globe.
High Patient Uptake for Text Message System Monitoring Opioid Use in Real-Time
Among the orthopaedic surgery patients in a study using text messaging to monitor opioid use, 61 percent of their tablets were found to be left over