Alcohol abuse is a serious problem worldwide. In England alone, over 350,000 alcohol-related hospital admissions – and over 5,000 alcohol-related deaths – were reported in 2018. Long-term alcohol abuse can have many harmful effects on our body. But one of the organs most affected by alcohol is the brain. Even moderate consumption changes brain structure and leads to cognitive issues, such as declines in memory and problem-solving.
Alcohol use is habit forming and can eventually lead to alcoholism. And though there are many treatments available for alcoholism, research shows these interventions often fail – with less than 20% of patients remaining alcohol free after intervention. Like every addiction, alcoholism is a disease and not a choice, so finding the root cause of it will make treatment easier.
Although genetics and the environment you live in are known to play a role in developing alcoholism, these factors don’t tell us how dependence occurs.
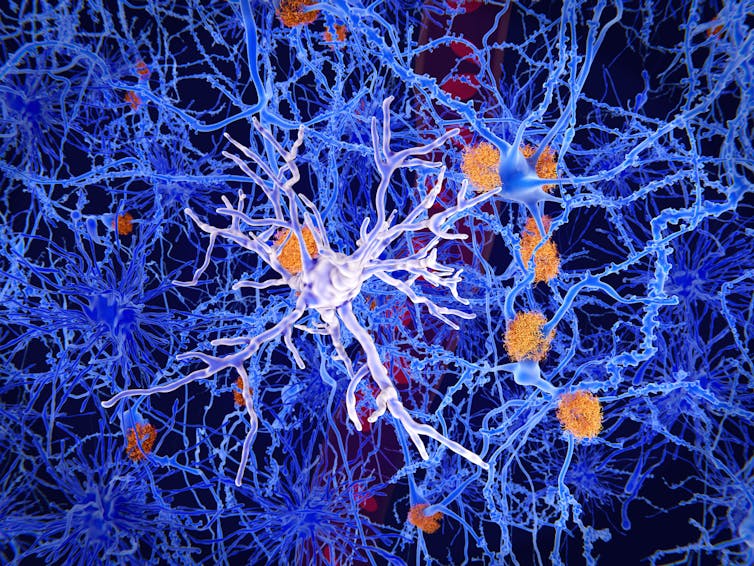
However, past research has found hints that the brain’s immune system cells (known as microglia) may be involved in addiction, including to cocaine and tobacco). One study even found that alcohol exposure and withdrawal in rats increased microglia numbers in the brain, before any other signs of alcohol-induced decline.
Another two recent studies have investigated brain changes seen in people and animals with alcohol dependence. Each of these studies found a common culprit: inflamed microglia.
Microglia are the brain’s resident immune system cells. Their main role is to guard and maintain balance in the brain. When microglia detect a threat, they respond by becoming inflamed and attacking. Normally, they return to normal after the threat is gone, but sometimes when inflammation becomes uncontrollable – such as with Alzeimer’s disease – it can lead to brain degeneration.
Microglia and addiction
One recent study used mice to study the effect of alcohol dependence on the brain.
In the brains of male mice that had alcohol dependency, research found there were more microglia cells in the medial prefrontal cortex, a region associated with pain, decision making, and memory processes. Similar results have also previously been found in humans.
They then examined what effects microglia depletion had on alcohol dependent mice by looking at their alcohol seeking behaviour, and anxious behaviour during alcohol withdrawal. The researchers found both factors were lowered when the microglia cells were reduced in the brain.
They also saw gene changes with microglia depletion. Genes involved in inflammation and immune responses were expressed less after depletion. The expression of genes involved in alcohol consumption, and alcohol dependence also changed when microglia had decreased. They also found that microglia depletion weakens brain circuits involved in the development of dependence and relapse behaviour in rodents.
A second study looking at both rodent and human brains also showed microglia is involved in alcohol dependence.
The researchers of this study used brain imaging, microglia depletion, and studies of post mortem brains, to examine changes that occur in alcohol dependence. For the brain imaging part, they used a variation of MRI scans, called DTI-MRI in humans and rats, focusing on a measure called mean diffusivity.
As DTI-MRI is based on the diffusion of water in tissues, mean diffusivity essentially shows the amount of diffusion of water molecules in tissues, with more dense and structurally-intact tissues having lower mean diffusivity. Mean diffusivity has previously been shown to change in the brain in inflammatory and degenerative conditions (including Alzheimer’s Disease and even psychosis). The researchers therefore chose to look at mean diffusivity as neuroinflammation is also involved in alcoholism. The researchers wanted to examine whether changes in mean diffusivity would be found between alcoholics and non-alcoholics, which hasn’t been done before.
Indeed their findings showed that mean diffusivity is overall higher in the brain of alcohol dependent rats and humans. They also found additional changes in how certain neurotransmitters – including dopamine, which is involved in alcohol dependence – move and are distributed in the brain.
The researchers went on to examine the microglia in the brains of rats with alcohol dependence, and rats with previous dependence who had abstained from alcohol for a week. They found a decreased amount of microglia in specific brain regions of dependent rats (including the hippocampus, which is involved in memory, and the nucleus accumbens, which is involved in the reward system). The microglia in the brains of alcohol dependent rats were also in their inflamed form.
Although this study showed a decrease in microglia numbers – whereas the previous study saw an increase – this might be because the researchers looked at different brain regions and used different research methods and animal models. However, both studies give hints towards how microglia functions during alcohol consumption and dependence, may differ in different brain regions.
The researchers also found that depleting microglia from the brain, or inducing microglia’s inflammatory response, led to similar results to each other, as both increased the mean diffusivity. Changes in microglia’s form when inflamed were also similar to the ones they observed in dependent rats. They concluded that the changes in the brain areas they studied could be explained by an inflammatory reaction of microglia caused by alcohol.
One limitation of both studies’ findings is that they used both only male rodents and male humans. However, both studies exhibit how alcoholism is a complex disease that produces clear changes in the brain.
Examining how exactly microglia is involved, and being able to interfere with their responses, could lead to better understanding and detection of addiction to alcohol, and give a good stepping stone for future targeted interventions.
