PASADENA — As Fernando Ramirez drove to work the day after the Eaton Fire erupted, smoke darkened the sky, ash and embers rained onto his windshield, and the air smelled of melting rubber and plastic.
He pulled to the side of the road and cried at the sight of residents trying to save their homes.
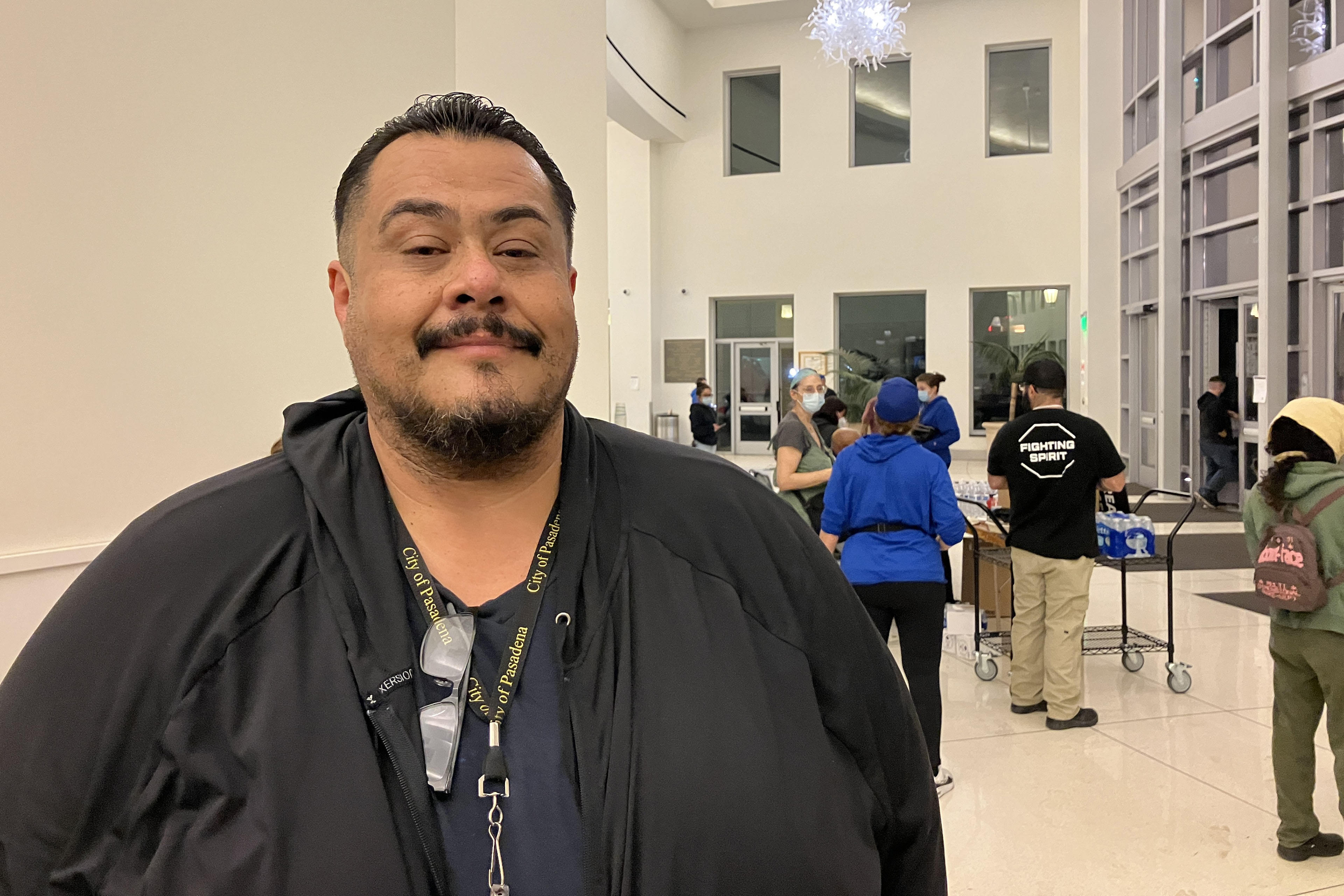
“I could see people standing on the roof, watering it, trying to protect it from the fire, and they just looked so hopeless,” said Ramirez, a community outreach worker with the Pasadena Public Health Department.
That evening, the 49-year-old volunteered for a 14-hour shift at the city’s evacuation center, as did colleagues who had also been activated for emergency medical duty. Running on adrenaline and little sleep after finding shelter for homeless people all day, Ramirez spent the night circulating among more than a thousand evacuees, offering wellness checks, companionship, and hope to those who looked distressed.
Local health departments, such as Ramirez’s, have become a key part of governments’ response to wildfires, floods, and other extreme weather events, which scientists say are becoming more intense and frequent due to climate change. The emotional toll of fleeing and possibly losing a home can help cause or exacerbate mental health conditions such as anxiety, depression, post-traumatic stress disorder, suicidal ideation, and substance use, according to health and climate experts.
Wildfires have become a recurring experience for many Angelenos, making it difficult for people to feel safe in their home or able to go about daily living, said Lisa Wong, director of the Los Angeles County Department of Mental Health. However, with each extreme weather event, the county has improved its support for evacuees, she said.
For instance, Wong said the county deployed a team of mental health workers trained to comfort evacuees without retraumatizing them, including by avoiding asking questions likely to bring up painful memories. The department has also learned to better track people’s health needs and redirect those who may find massive evacuation settings uncomfortable to other shelters or interim housing, Wong said. In those first days, the biggest goal is often to reduce people’s anxiety by providing them with information.
“We’ve learned that right when a crisis happens, people don’t necessarily want to talk about mental health,” said Wong, who staffed the evacuation site Jan. 8 with nine colleagues.
Instead, she and her team deliver a message of support: “This is really bad right now, but you’re not going to do this alone. We have a whole system set up for recovery too. Once you get past the initial shock of what happened — initial housing needs, medication needs, all those things — then there’s this whole pathway to recovery that we set up.”
The convention center in downtown Pasadena, which normally hosts home shows, comic cons, and trade shows, was transformed into an evacuation site with hundreds of cots. It was one of at least 13 shelters opened to serve more than 200,000 residents under evacuation orders.

The January wildfires have burned an estimated 64 square miles — an area larger than the city of Paris — and destroyed at least 12,300 buildings since they started Jan. 7. AccuWeather estimates the region will likely face more than $250 billion in economic losses from the blazes, surpassing the estimates from the state’s record-breaking 2020 wildfire season.
Lisa Patel, executive director of the Medical Society Consortium on Climate and Health, said she’s most concerned about low-income residents, who are less likely to access mental health support.
“There was a mental health crisis even before the pandemic,” said Patel, who is also a clinical associate professor of pediatrics at Stanford School of Medicine, referring to the covid-19 pandemic. “The pandemic made it worse. Now you lace in all of this climate change and these disasters into a health care system that isn’t set up to care for the people that already have mental health illness.”
Early research suggests exposure to large amounts of wildfire smoke can damage the brain and increase the risk of developing anxiety, she added.
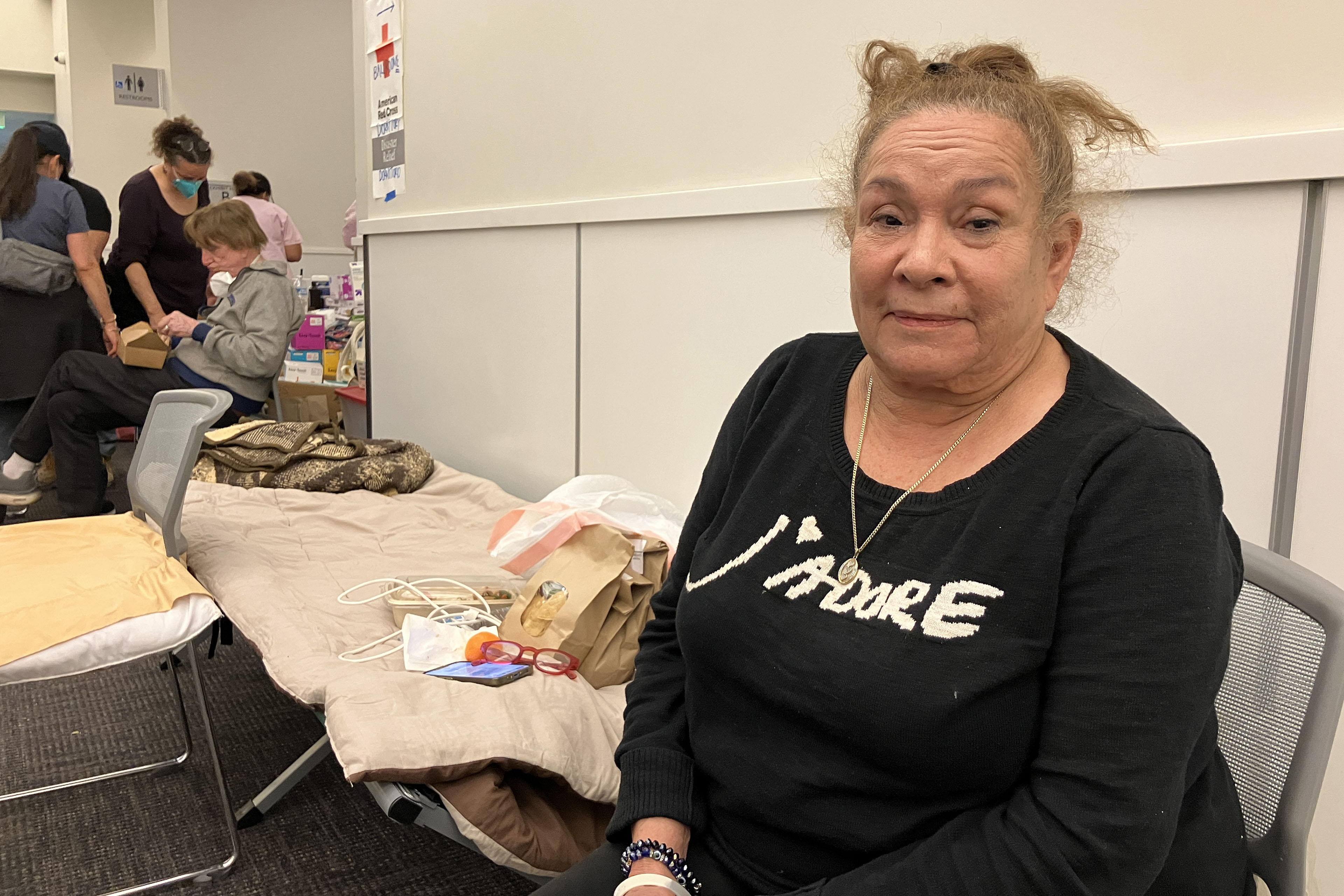
At the Pasadena Convention Center, Elaine Santiago sat on a cot in a hallway as volunteers pulled wagons loaded with soup, sandwiches, bottled water, and other necessities.
Santiago said she drew comfort from being at the Pasadena evacuation center, knowing that she wasn’t alone in the tragedy.
“It sort of gives me a sense of peace at times,” Santiago said. “Maybe that’s weird. We’re all experiencing this together.”
She had been celebrating her 78th birthday with family when she fled her home in the small city of Sierra Madre, east of Pasadena. As she watched flames whip around her neighborhood, she, along with children and grandkids, scrambled to secure their dogs in crates and grabbed important documents before they left.
The widower had leaned on her husband in past emergencies, and now she felt lost.
“I did feel helpless,” Santiago said. “I figured I’m the head of the household; I should know what to do. But I didn’t know.”
Donny McCullough, who sat on a neighboring green cot draped in a Red Cross blanket, had fled his Pasadena home with his family early on the morning of Jan. 8. Without power at home, the 68-year-old stayed up listening for updates on a battery-powered radio. His eyes remained red from smoke irritation hours later.
“I had my wife and two daughters, and I was trying not to show fear, so I quietly, inside, was like, ‘Oh my God,’” said McCullough, a music producer and writer. “I’m driving away, looking at the house, wondering if it’s going to be the last time I’m going to see it.”
He saved his master recording from a seven-year music project, but he left behind his studio with all his other work from a four-decade career in music.
Not all evacuees arrived with family. Some came searching for loved ones. That’s one of the hardest parts of his shift, Ramirez said. The community outreach worker helped walk people around the building, cot by cot.
A week in, at least two dozen people had been killed in the wildfires.
The work takes a toll on disaster relief workers too. Ramirez said many feared losing their homes in the fires and some already had. He attends therapy weekly, which he said helps him manage his emotions.
At the evacuation center, Ramirez described being on autopilot.
“Some of us react differently. I tend to go into fight mode,” Ramirez said. “I react. I run towards the fire. I run towards personal service. Then once that passes, that’s when my trauma catches up with me.”
Need help? Los Angeles County residents in need of support can call the county’s mental health helpline at 1-800-854-7771. The national Suicide & Crisis Lifeline, 988, is also available for those who’d like to speak with someone confidentially, free of charge.










