GREELEY, Colorado — A principios de agosto, trabajadores agrícolas se reunieron en un parque de Greeley para celebrar con un picnic el Día de Apreciación del Trabajador Agrícola. Un signo de que este año fue diferente de los anteriores fue el menú: fajitas de res, tortillas, pico de gallo, chips, frijoles… pero sin pollo.
Las granjas en Colorado habían sacrificado a millones de pollos en los últimos meses para detener la transmisión de la gripe aviar. Los organizadores completaron la oferta con perritos calientes.
Sin importar el menú, algunos trabajadores de tambos en el evento dijeron que no se sienten exactamente “apreciados”. Dijeron que no han recibido ningún equipo de protección personal más allá de guantes para protegerse contra el virus, incluso cuando ellos o sus compañeros han tenido conjuntivitis y síntomas parecidos a la gripe que temen que sea gripe aviar.
“Deberían darnos algo más”, dijo en español un trabajador del condado de Larimer. Habló bajo condición de anonimato por miedo a perder su trabajo por hablar. “¿Qué pasa si nos sucede algo? Actúan como si no pasara nada”.
Expertos en salud y seguridad agrícola han estado tratando de difundir información sobre cómo protegerse contra la gripe aviar, incluso a través de videos bilingües en TikTok que muestran la manera correcta de equiparse con respiradores, protección ocular, guantes y overoles. Y los departamentos de salud y agricultura de Colorado han ofrecido un suministro gratuito de un mes de equipo de protección a cualquier productor que lo solicite.
Pero hasta ahora, muchas granjas no lo han solicitado: según cifras proporcionadas por el departamento de salud del estado a finales de agosto, menos del 13% de los tambos del estado habían solicitado y recibido estos equipos.
Se sabe que el virus infecta a mamíferos, desde zorrinos, osos y vacas hasta personas y mascotas. Comenzó a aparecer en ganado lechero en los últimos meses, y Colorado ha sido uno de los estados más afectados. Diez de los 13 casos humanos confirmados en este año en el país han ocurrido en Colorado, donde sigue circulando entre las vacas lecheras. No es un riesgo en carne cocida o leche pasteurizada, pero es riesgoso para quienes entran en contacto con animales infectados o leche cruda.
El condado de Weld, donde se celebró el evento para los trabajadores agrícolas, es uno de los principales productores de leche del país, suministrando suficiente leche cada mes este año como para llenar unas 45 piscinas olímpicas, según datos del Departamento de Agricultura de Estados Unidos. Los condados vecinos también son productores destacados.
Cada vez hay más preocupación sobre enfermedades no diagnosticadas entre los trabajadores agrícolas debido a la falta de pruebas y precauciones de seguridad.

Otra razón para preocuparse: la gripe aviar y la gripe estacional son capaces de intercambiar genes, por lo que si “conviven” el mismo cuerpo al mismo tiempo, la gripe aviar podría terminar con genes que aumenten su capacidad de contagio. Aún no parece que el virus se esté propagando fácilmente entre personas. Pero eso podría cambiar, y si no se están realizando pruebas, los funcionarios de salud podrían tardar en darse cuenta.
Las cepas de la gripe estacional ya matan a unas 47,000 personas en el país cada año. Los funcionarios de salud pública temen el caos que una nueva forma de gripe podría causar si se propaga entre las personas.
Los Centros para el Control y Prevención de Enfermedades (CDC) recomiendan que los trabajadores en tambos usen un respirador y gafas o protección facial, entre otras protecciones, ya sea que estén trabajando con animales enfermos o no.
Un estudio reciente encontró que no todas las vacas infectadas muestran síntomas, por lo que los trabajadores podrían estar en contacto con animales contagiosos sin darse cuenta.
Incluso cuando se sabe que los animales están infectados, a menudo los trabajadores agrícolas aún tienen que estar en contacto cercano con ellos, a veces bajo condiciones agotadoras, como durante una reciente ola de calor cuando los trabajadores avícolas de Colorado recogieron cientos de pollos a mano para sacrificarlos debido al brote. Al menos seis de los trabajadores se infectaron con la gripe aviar.
Un trabajador lechero en el condado de Weld, que habló de manera anónima por miedo a perder su trabajo, dijo que su empleador no ha ofrecido ningún equipo de protección más allá de los guantes, a pesar de que trabaja con vacas enfermas y leche cruda.
Sus jefes pidieron a los trabajadores que separaran las vacas enfermas de las demás después de que algunas produjeran menos leche, perdieran peso y mostraran signos de debilidad, dijo. Pero el empleador no mencionó nada sobre la gripe aviar, ni sugirió que tomaran precauciones para protegerse.
Dijo que, a principios de este verano, se compró gafas protectoras en Walmart cuando sus ojos se pusieron rojos y comenzaron a picarle. Recordó haber tenido mareos, dolores de cabeza y falta de apetito en la misma época. Pero se automedicó y siguió adelante, sin faltar al trabajo ni ir al médico.
“Tenemos que protegernos porque nunca se sabe”, dijo en español. “Le digo a mi esposa e hijo que las vacas están enfermas, y ella me dice que me vaya, pero será lo mismo dondequiera que vaya”.
Dijo que había oído que sus empleadores no eran comprensivos cuando un colega les dijo que se sentía enfermo. Incluso vio a alguien relacionado con la gerencia quitar un volante sobre cómo las personas pueden protegerse de la gripe aviar y tirarlo a la basura.
El trabajador lechero en el condado vecino de Larimer dijo que él también solo ha tenido guantes como protección, incluso cuando ha trabajado con animales enfermos, lo suficientemente cerca como para que la saliva se le pegue. Comenzó a trabajar con ellos cuando un colega faltó al trabajo por tener síntomas similares a la gripe: fiebre, dolor de cabeza y ojos rojos.
“Solo uso guantes de látex”, dijo. “Y veo que los que trabajan con las vacas que están enfermas también solo usan guantes”.
Dijo que, en el trabajo, no tiene tiempo para lavarse las manos, pero se pone desinfectante de manos antes de irse a casa y se ducha una vez que llega. No ha tenido síntomas de infección.
Estos relatos de trabajadores en tambos son similares a los de trabajadores agrícolas en Texas, según informó KFF Health News en julio.
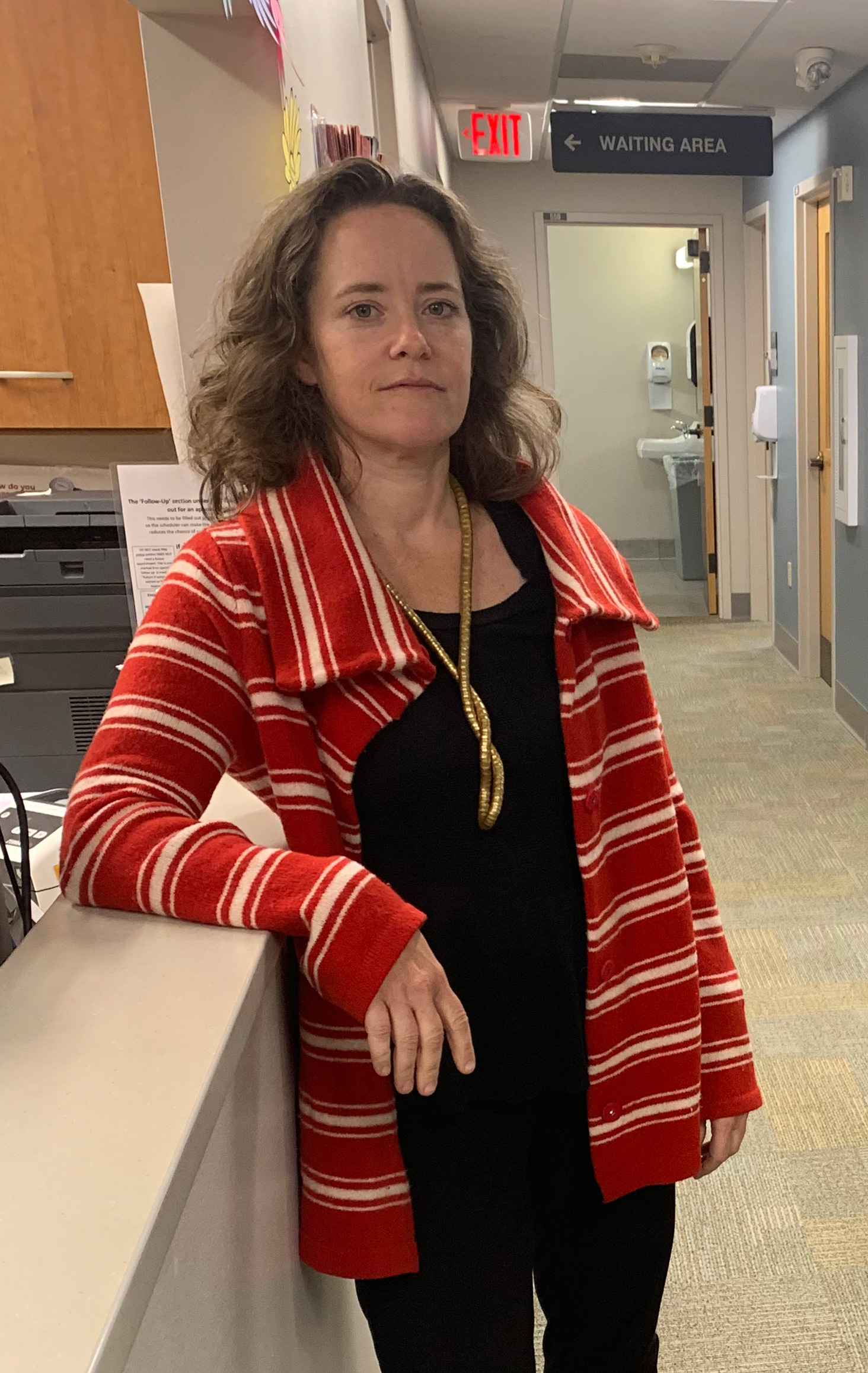
“Los empleadores que están siendo proactivos y están proporcionando EPP parecen ser la minoría en la mayoría de los estados”, dijo Bethany Boggess Alcauter del Centro Nacional de Salud para Trabajadores Agrícolas, una organización sin fines de lucro con sede en Texas que aboga por mejorar la salud de los trabajadores agrícolas y de sus familias. “Los trabajadores agrícolas están recibiendo muy poca información”.
Pero Zach Riley, director ejecutivo de la Asociación de Ganaderos de Colorado, dijo que cree que esos escenarios son la excepción, no la regla.
“Sería difícil encontrar una operación lechera que no esté proporcionando ese EPP,” dijo. Riley agregó que las granjas típicamente tienen un stock de EPP listo para situaciones como esta y que, si no lo tienen, es fácil de conseguir a través del estado. “Solo tienes que pedirlo”.
Los productores están muy motivados para mantener las infecciones bajo control, dijo, porque “la leche es su fuente de vida”. Apuntó que ha escuchado de algunos productores que “sus familiares que trabajan en la granja están haciendo jornadas de 18 a 20 horas solo para tratar de mantenerse al frente, para que sean la primera línea entre todo, para proteger a sus empleados”.
El Departamento de Salud de Colorado está anunciando una línea directa que los trabajadores en tambos enfermos pueden llamar para obtener ayuda para hacerse una prueba de gripe y recibir medicamentos.
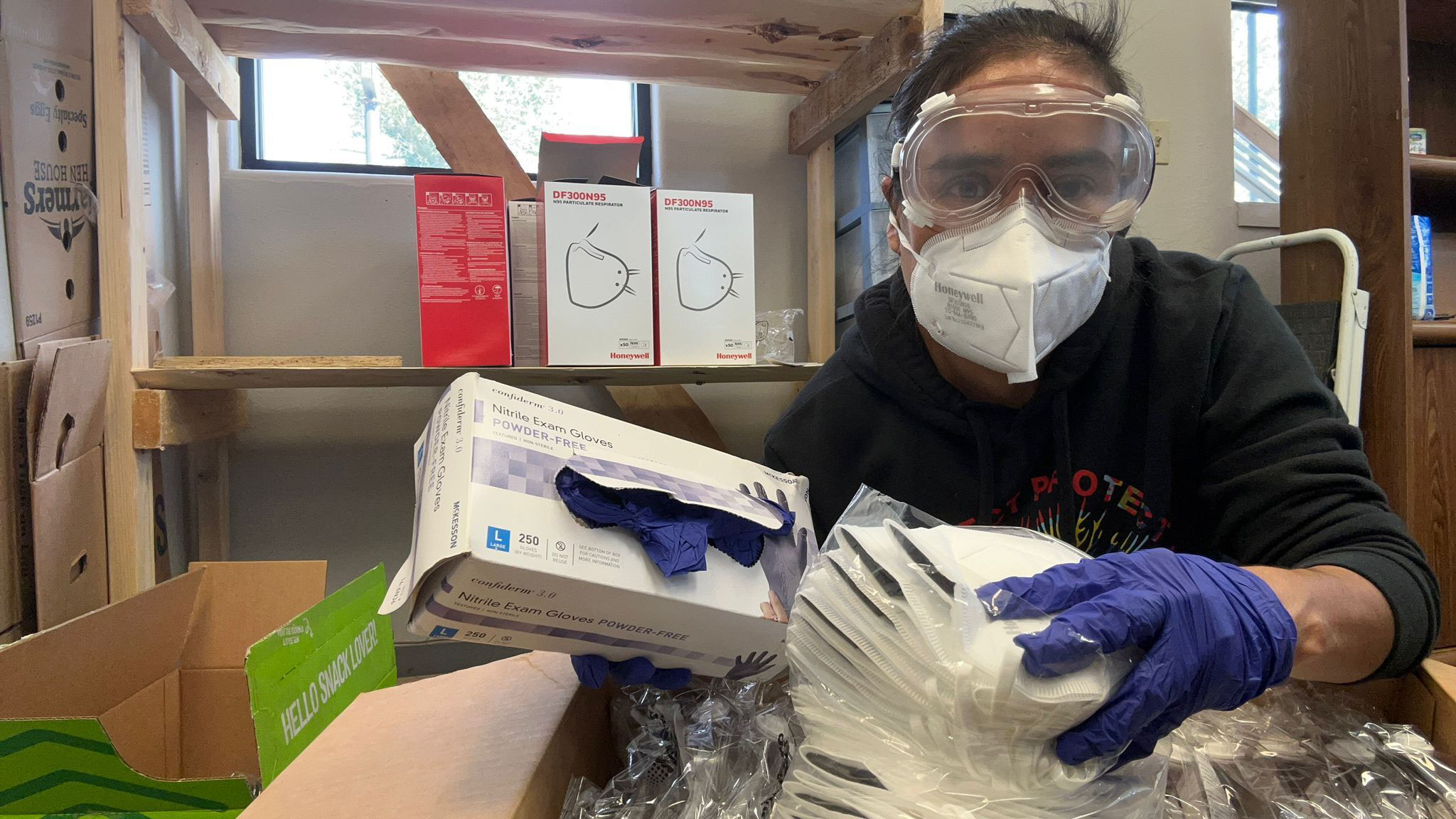
Project Protect Food Systems Workers, una organización que surgió a principios de la pandemia de covid-19 para promover la salud de los trabajadores agrícolas en todo Colorado, está distribuyendo EPP que recibió del estado para que promotoras, trabajadores de salud que son parte de la comunidad a la que ayudan, puedan distribuir máscaras y otras protecciones directamente a los trabajadores si los empleadores no las están proporcionando.
La promotora Tomasa Rodríguez dijo que los trabajadores “lo ven como otro virus, otro covid, pero es porque no tienen suficiente información”.
Ha estado repartiendo volantes sobre síntomas y medidas de protección, pero no puede acceder a muchos tambos. “Y en algunos casos, muchos de estos trabajadores no saben leer, por lo que los volantes no les llegan, y luego los empleadores no están haciendo ningún tipo de charlas o capacitaciones”, dijo.
Nirav Shah de los CDC dijo durante una llamada con periodistas el 13 de agosto que la concientización sobre la gripe aviar entre los trabajadores en granjas lecheras no es tan alta como a los funcionarios les gustaría, a pesar de meses de campañas en redes sociales y estaciones de radio.
“Todavía queda un camino por recorrer para que la concientización esté al nivel que podría estar en el mundo avícolas”, dijo. “Estamos utilizando todas las vías de comunicación que podemos”.
Los corresponsales de KFF Health News Vanessa G. Sánchez y Amy Maxmen contribuyeron con este informe.
Healthbeat es una redacción sin fines de lucro que cubre temas de salud pública, publicada por Civic News Company y KFF Health News. Suscríbete a sus newsletters aquí.
Esta historia fue producida por KFF Health News, conocido antes como Kaiser Health News (KHN), una redacción nacional que produce periodismo en profundidad sobre temas de salud y es uno de los principales programas operativos de KFF, la fuente independiente de investigación de políticas de salud, encuestas y periodismo.