Donald Trump could have destroyed the Affordable Care Act, but “he chose to build upon [it].”
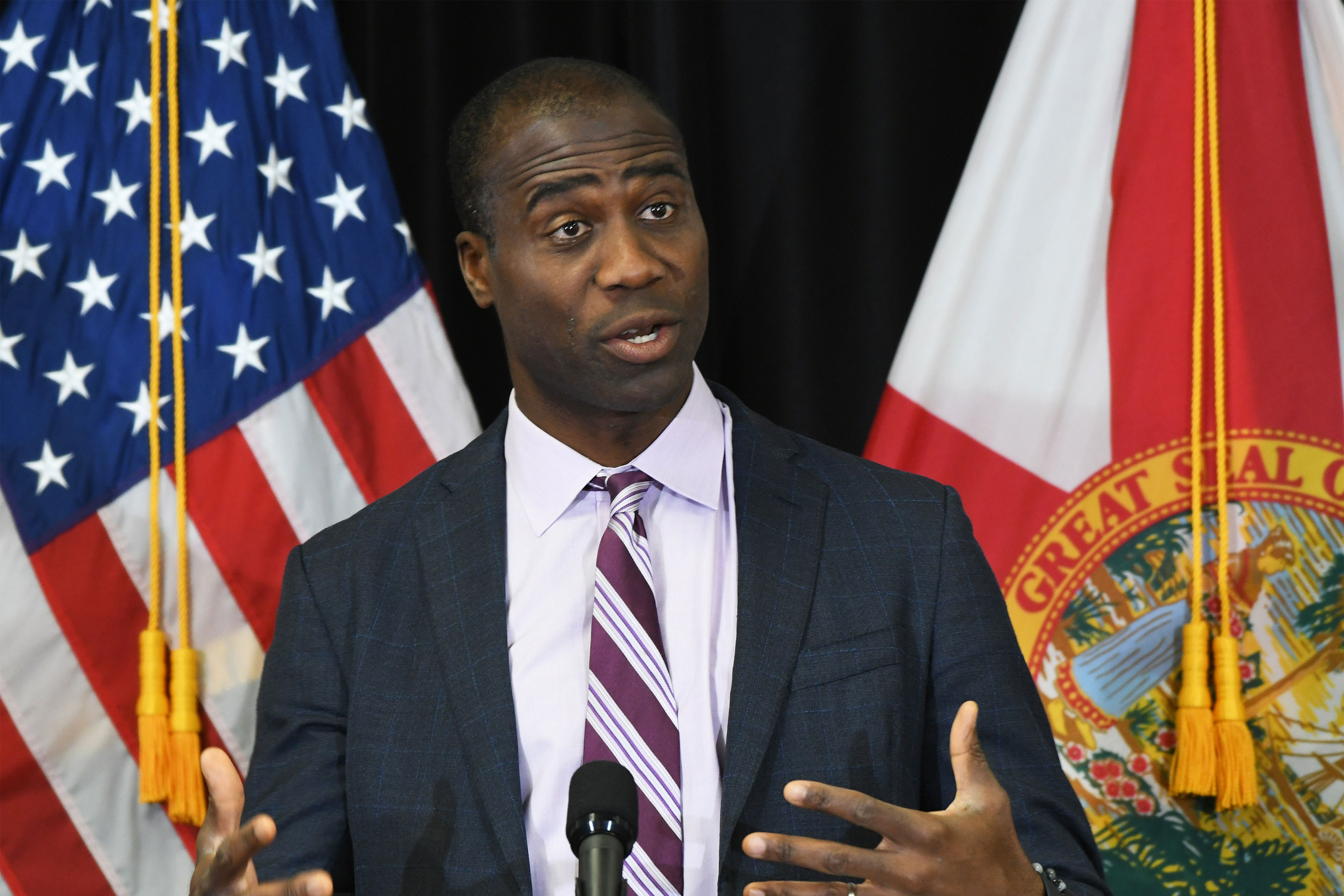
Sen. JD Vance (R-Ohio) on “Meet the Press,” Sept. 15
Sen. JD Vance (R-Ohio) on Sept. 15 told viewers of NBC’s “Meet the Press” that former President Donald Trump built up the Affordable Care Act, even though Trump could have chosen to do the opposite.
“Donald Trump had two choices,” Vance, Trump’s running mate, said. “He could have destroyed the program, or he could actually build upon it and make it better so that Americans didn’t lose a lot of health care. He chose to build upon a plan, even though it came from his Democratic predecessor.”
The remarks follow statements the former president made during his Sept. 10 debate with Vice President Kamala Harris in Philadelphia. Trump said of the ACA, “I saved it.”
The Affordable Care Act, aka Obamacare, has grown more popular as Americans have increasingly used it to gain health coverage. More than 20 million people enrolled this year in plans sold through the marketplaces it created. That makes the law a tricky political issue for Republicans, who have largely retreated from their attempts over the past decade to repeal it.
Both Vance’s and Trump’s statements are false. We contacted Vance’s campaign; it provided no additional information. But here’s a review of policies related to Obamacare that Trump pursued as president.
So What Did Trump Do With the ACA?
Most of the Trump administration’s ACA-related actions involved cutting the program, including reducing by millions of dollars funding for marketing and enrollment assistance and backing the many failed efforts in Congress and the courts to overturn the law. In June 2020, for example, the administration asked the Supreme Court to overturn the law in a case brought by more than a dozen GOP states. The high court eventually rejected the case.
“The fact the ACA survived the Trump administration is a testament to the strength of the underlying statutory framework, and that the public rallied around it,” said Sabrina Corlette, co-director of the Center on Health Insurance Reforms at Georgetown University.
Most ACA provisions took effect in 2014, during Barack Obama’s presidential administration.
Average premium costs, already rising when Trump took office, jumped for some plans in 2018, before beginning a modest decline for the rest of his term, according to statistics from KFF, a health information nonprofit that includes KFF Health News.
Some of those increases were tied to a 2017 Trump administration decision to stop making payments to insurers, which was intended to reduce deductibles and copayments for people with low to moderate incomes. By law, though, insurers still had to offer the plans.
Two months earlier, the Congressional Budget Office warned that stopping the payments could cause some insurers to leave the ACA marketplace — and that premiums would rise by 20% in the first year.
Most states, however, let insurers make up for the lost payments by increasing monthly premiums. That had the unintended effect of boosting federal subsidies for people who buy Obamacare plans, because the subsidies are tied to the cost of premiums.
“By accident, that gave people cheaper access to better coverage in the exchange plans,” said Joe Antos, a senior fellow emeritus with the American Enterprise Institute.
Some Republicans think Trump deserves credit for this inadvertent improvement.
But Larry Levitt, KFF’s executive vice president for health policy, said that wasn’t the Trump administration’s intention.
“The one time when Trump improved the ACA, it was an unintended consequence of an attempt to weaken it,” he said.
Meanwhile, the Trump administration expanded access to some kinds of less expensive health coverage that aren’t compliant with ACA rules, including short-term plans that generally have more restrictions on care and can leave consumers with surprise medical bills. Democrats call the plans “junk insurance.”
Brian Blase, president of the Paragon Health Institute, a conservative health research group, said broader access to cheaper, less comprehensive plans helped more people get coverage. The plans’ critics say that if they had attracted too many healthy people from ACA-compliant insurance, increases could have spiked for people who remained.
Trump also supported congressional repeal-and-replace efforts, all of which failed — including on the memorable night when Sen. John McCain (R-Ariz.) helped kill the effort with a thumbs-down vote. The Trump administration never issued its own replacement plan, despite the former president’s many promises that he would.
Trump, during the debate with Harris, said that he has “concepts of a plan” to replace Obamacare and that “you’ll be hearing about it in the not-too-distant future.”
On “Meet the Press,” host Kristen Welker asked Vance when Trump’s plan would be ready. He didn’t answer directly but said it would involve “deregulating the insurance market.”
Critics say that’s code for letting insurers do business as they did pre-ACA, when sick people could be denied coverage or charged exorbitant premiums based on preexisting conditions.
Our Ruling
Vance’s assertion that Trump as president took steps to build upon the ACA and protect the health coverage of 20 million Americans is simply not supported by the record.
Trump administration policies, for example, didn’t buttress the ACA but often undermined enrollment outreach efforts or were advanced to sabotage the insurance marketplace. Also, Trump vocally supported congressional efforts to overturn the law and legal challenges to it.
By the numbers, Affordable Care Act enrollment declined by more than 2 million people during Trump’s presidency, and the number of uninsured Americans rose by 2.3 million, including 726,000 children, from 2016 to 2019, according to the U.S. Census Bureau. That includes nearly three years of Trump’s presidency.
We rate Vance’s statement False.
SOURCES:
“Meet the Press” interview with Sen. JD Vance, Sept. 15, 2024.
Brookings Institution, “Six Ways Trump Has Sabotaged the Affordable Care Act,” Oct. 9, 2020.
Vox, “Trump Is Slashing Obamacare’s Advertising Budget by 90%,” Aug. 31, 2017.
Center on Budget and Policy Priorities, “Trump Administration Has Cut Navigator Funding by Over 80 Percent Since 2016,” Sept. 13, 2018.
The New York Times, ‘Trump Administration Asks Supreme Court To Strike Down Affordable Care Act,” June 26, 2020.
Constitutional Accountability Center, Texas v. United States, accessed Sept. 16, 2024.
Harvard T.H. Chan School of Public Health, “Quantifying Health Coverage Losses Under Trump,” Nov. 3, 2020.
Center on Budget and Policy Priorities, “Uninsured Rate Rose Again In 2019, Further Eroding Earlier Progress,” Sept. 15, 2020.
U.S. Census Bureau, Health Insurance Historical Tables, revised Aug. 22, 2024.
KFF, Marketplace Average Benchmark Premiums, accessed Sept. 16, 2024.
Brookings Institution, “The Case for Replacing ‘Silver Loading,’” May 20, 2021.
KFF Health News, “Trump Administration Loosens Restrictions on Short-Term Health Plans,” Aug. 1, 2018.
The New York Times, “Biden Administration Finalizes Rule Curbing Use of Short-Term Health Plans,” March 28, 2024.
Telephone interview, Sabrina Corlette, co-director of the Center on Health Reforms at Georgetown University, Sept. 16, 2024.
Telephone interview, Joe Antos, senior fellow emeritus, American Enterprise Institute, Sept. 16, 2024.
Email correspondence, Brian Blase, president of the Paragon Health Institute, Sept. 16, 2024.
Email correspondence, Larry Levitt, KFF executive vice president for health policy, Sept. 18, 2024.
Congressional Budget Office, “The Effects of Terminating Payments for Cost-Sharing Reductions,” Aug. 15, 2017.
USA Today, “Trump To End Cost-Sharing Subsidies to Insurance Companies,” Oct. 12, 2017.
New York magazine, “Vance: Trump’s Health-Care Plan Is To Let Insurers Charge More for Preexisting Conditions,” Sept. 17, 2024.
This article was produced by KFF Health News, a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.