Ann Lewandowski knows all about pharmacy benefit managers, or PBMs, the companies that shape the U.S. drug market. Her job, as a policy advocate at drugmaker Johnson & Johnson, was to tell patient and physician groups about the PBMs’ role in high drug prices.
Armed with that knowledge, Lewandowski filed a potentially groundbreaking lawsuit in February. Rather than targeting the PBMs, however, she went after a big company that uses one — her own employer, Johnson & Johnson.
Lewandowski charges in her lawsuit that by contracting with the PBM Express Scripts, which is part of the insurance giant Cigna, Johnson & Johnson — which fired her in April — failed in its duty to ensure reasonable drug prices for its more than 50,000 U.S. employees.
By choosing an Express Scripts plan, she charged, J&J cost employees “millions of dollars in the form of higher payments for prescription drugs, higher premiums, higher deductibles, higher coinsurance, higher copays, and lower wages or limited wage growth.”
Lewandowski, 40, from outside Madison, Wisconsin, relies on an expensive multiple sclerosis drug. She brought the lawsuit, she said, because she “had trouble aligning the policy positions” she reported on as a J&J employee “with the actions I experienced as a health plan user.”
In recent years, the opaque business practices of PBMs have drawn fire. The Federal Trade Commission is conducting a lengthy investigation of the three biggest companies and sued them in September, accusing the firms of driving up insulin prices. Bipartisan bills in Congress would rein them in. And businesses such as Mark Cuban’s Cost Plus Drugs and smaller, “transparent PBMs” have tried to wean pharmaceutical companies and health plans from their reliance on the big PBMs.
But Lewandowski’s lawsuit goes to a sensitive spot that had been overlooked until recently: language in the 2021 appropriations bill that revised the 1974 Employee Retirement Income Security Act, known as ERISA. The original law focused on stopping fraudulent retirement plans.
Her lawsuit is based on congressional language specifying that the law’s requirement of prudent management covers health as well as retirement benefits. By providing workers with a health plan, employers aren’t “doing you a favor. They are holding your money and investing it in your health,” said Barak Richman, a George Washington University health law professor.
In July, a similar lawsuit was filed against Wells Fargo, and more suits are in the works.
PBMs demand discounts and rebates from drugmakers, which leads the manufacturers to charge higher list prices, which can drive up the price patients pay at the pharmacy. At the same time, retail pharmacies say PBMs are driving them out of business by paying them less than what the PBMs charge health plans — a practice known as spread pricing. Patients typically have no idea what they’ll pay for a drug, and neither do their employers, because many PBMs’ contracts contain nondisclosure clauses.
Dissatisfaction with the status quo and fear of liability are pushing employers to switch from the “Big Three” PBMs to “transparent PBMs,” which don’t shroud their pricing and drug choice decisions.
“We brought on nine Fortune 500s this year, 1.2 million patients,” said AJ Loiacono, CEO of New York City-based Capital Rx, a PBM founded in 2017. According to a recent survey, as many as half of U.S. employers are considering switching.
Cuban, in an interview with KFF Health News, said he has told hundreds of Fortune 500 executives, in one-on-one meetings and in groups, that they are overpaying on drug benefit plans skewed to fatten the wallets of big PBMs.
“You’re getting ripped off,” Cuban said he tells them. “You don’t really understand the elements, and that’s costing you money and costing you wellness. And now you are going to get sued. It’s not a question of if but a question of when.”
Pressuring a Purchasing Cartel
The billionaire, who launched Mark Cuban Cost Plus Drugs in 2022 to upend the byzantine $500 billion U.S. drug market, is convinced that the Lewandowski suit and others will end the dominance of the big PBMs, which control 80% of the business.
Cost Plus Drugs charges a straight 15% markup with small processing fees for the 2,500 drugs it sells, most of them generics, said co-founder Alex Oshmyansky. Its nearly 3 million customers — individuals, health plans, and transparent PBMs — appear to be saving money in many cases.
The big PBMs say their buying power and exclusive access to information enable them to save money for insurers, employers, and patients. Critics say they are skimming up to 25% from the drug market, perhaps $100 billion a year, according to Oshmyansky. The opaque strategies and conflicts of interest, critics say, often result in the poorest, sickest patients paying the most for medications.
The three PBMs amount to a “purchasing cartel,” Oshmyansky said in an interview at Cost Plus’ Dallas headquarters, once the office of broadcast.com, the internet radio company that made Cuban his first billion dollars when he sold it to Yahoo in 1999. “They buy all the drugs, they jack up the prices, and then they resell them.”
Richman and Amy Monahan of the University of Minnesota argued in a journal article this year that the Department of Labor, which has previously focused its ERISA oversight on retirement benefits, should issue standards for the use of health care dollars under the law.
When companies “enter into dumb contracts with insurers or PBMs, arguably they are in violation of ERISA,” Richman said. “Taking the law seriously would really require employers, who are spending half the health care dollars in the country, to spend that money in very different ways.”
Some drug market experts, however, doubt the ERISA lawsuits will succeed. Complex PBM money channels “make it hard to build a case,” said Stacie Dusetzina, a professor of health policy at Vanderbilt University School of Medicine. “You might think your company is overpaying, but relative to what?”
The ERISA Industry Committee, which lobbies Congress for some of the biggest U.S. companies, is asking Congress to give PBMs the specific duty to represent their clients’ financial interests, said Melissa Bartlett, the group’s senior vice president for health policy. That could require patients to sue the PBMs rather than their employers.
A few big employers are already changing their drug plans.
In 2019, Connecticut became CVS’ first PBM customer to negotiate a transparent fee structure. Its contract required 100% of drug rebates be passed along to the state and eliminated spread pricing.
The state decided to go further when it sought a new contract for its 214,000 employees this year, said Joshua Wojcik, director of health policy and benefits in the state comptroller’s office. Instead of discounts and rebates, it demanded the lowest net cost per employee.
Of the three big PBMs, only CVS bid on the contract. It edged out a few “transparent PBMs” — a sign, in Wojcik’s view, that CVS at least doesn’t want to be left out as more customers ditch the current PBM business model.
With the change, Wojcik estimates the state will save up to $70 million a year.
$13.40 vs. $2,500
Changing drug benefit policies at big companies takes time, said Oshmyansky of Cost Plus. Their PBM contracts last three to five years, so “you have to capture them in that one year where they are evaluating other options,” he said. PBMs pay benefit plan consultants and the brokers big companies hire to steer business their way.
“We have this weird structure where multiple sclerosis, cancer patients subsidize everybody else’s drugs,” Oshmyansky said. Instead of creating a pool that spreads costs to everyone with insurance, there’s a “disproportionate burden placed on the sickest members.”
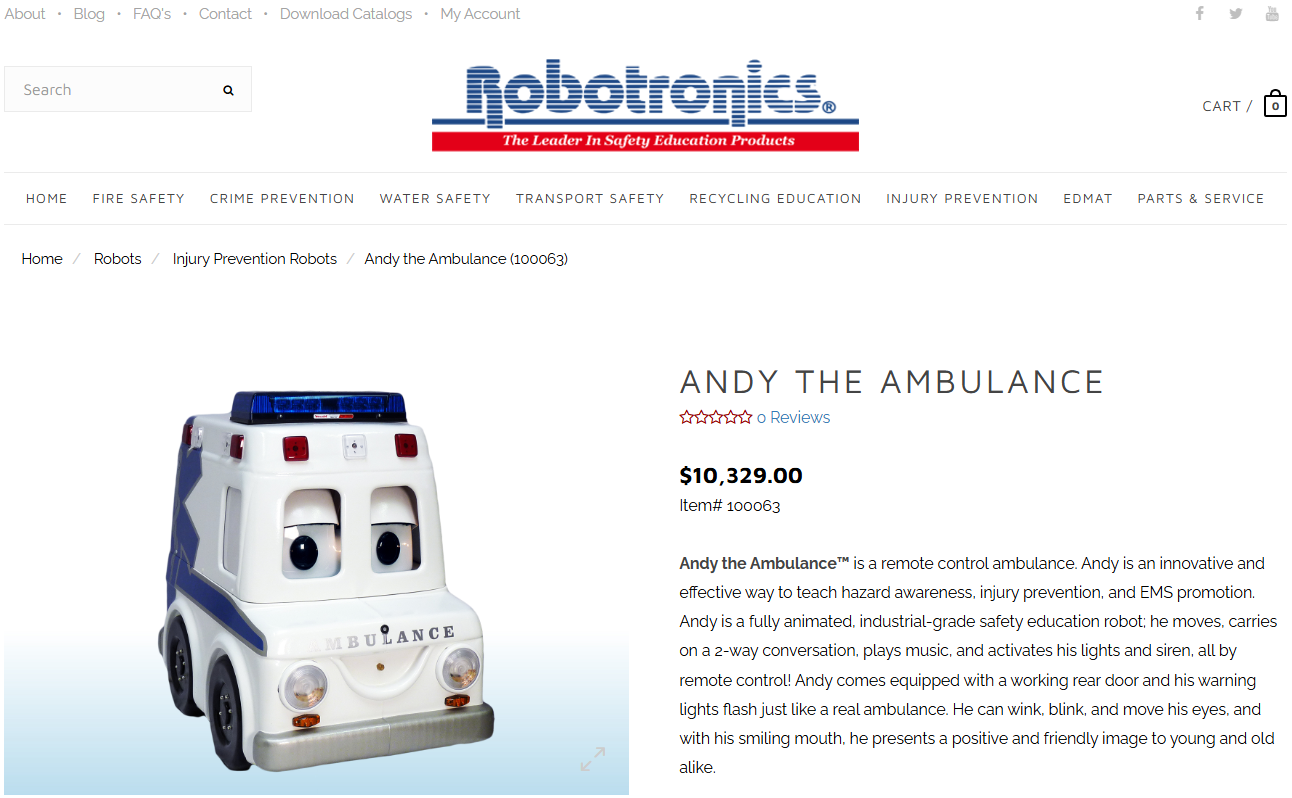
Cost Plus generates the biggest savings for its customers on about 50 extraordinarily high-priced generic drugs. The poster child is imatinib, a generic cancer pill that Cost Plus sells for $13.40 for a 30-day supply, compared with the $2,500 it retails for at pharmacies. A study conducted by Dusetzina and colleagues found Medicare could save $662 million a year just by buying imatinib and six other generic cancer drugs from Cost Plus rather than through a big PBM.
Ironically, though, most generic drugs are cheaper in the U.S. than in Europe or Canada — so cheap, in fact, that they fall into shortages as companies get out of the business or stop making needed improvements to their production lines.
In response, Cost Plus has started a compounding pharmacy to make common generics and soon hopes to have a sort of “private reserve” of 70 to 80 products that it can make on short notice if they go into shortage, Oshmyansky said.
While the company hasn’t yet set up purchase agreements for most brand-name drugs, Oshmyansky and Cuban are hopeful. Drugmakers, through their trade group Pharmaceutical Research and Manufacturers of America, have lobbied fiercely to rein in PBMs in the past two years.
At a Sept. 24 hearing at which Sen. Bernie Sanders (I-Vt.) grilled Novo Nordisk CEO Lars Fruergaard Jørgensen over high prices for diabetes and weight loss drugs Ozempic and Wegovy, the executive expressed support for a more transparent pricing model.
“On average for our products we give 74% in rebates to PBMs” for every $1 the company charges, he said. If, instead, “we simply paid the PBMs a small fee for the limited risk and contribution they make, I think patients would be significantly better off.”
This article was produced by KFF Health News, a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.