By Bill White
Posted on his website, Selected Papers of William L. White, on October 1, 2020
In my early writings on the history of addiction in the United States, I document the discrepancy between public perception of substance-related problems and data documenting the actual patterns of such problems. For example, the sensationalist 1960s media coverage in the United States of marijuana and LSD use obscured fundamental shifts in alcohol, tobacco, and prescription drug use in the U.S. Lowered age of onset of alcohol use, increased alcohol and tobacco consumption among women, and the increased prevalence of prescription drug dependence remained invisible amidst lurid tales of illicit counterculture drug use.
Two recent studies raise similar concerns that panic over recent drug surges (e.g., methamphetamines and opioids) may be similarly obscuring intensified surges in alcohol consumption and its related consequences.
In the first study, White and colleagues (2020) use data from the National Center for Health Statistics to analyze trends in alcohol-related mortality in the U.S. between 1999 and 2017. Their major findings include the following:
-
The number of alcohol-related deaths per year among people aged 16+ doubled from 35,914 to 72,558 (a rate increase of 50.9%).
-
Nearly 1 million alcohol-related deaths (944,880) were recorded between 1999 and 2017.
-
In 2017, 2.6% of roughly 2.8 million deaths in the United States involved alcohol. Nearly half of alcohol-related deaths resulted from liver disease (30.7%; 22,245) or overdoses on alcohol alone or with other drugs (17.9%; 12,954).
-
Rates of alcohol-related deaths were highest among males, people in age-groups spanning 45 to 74 years, and among non-Hispanic (NH) American Indians or Alaska Natives.
-
Rates increased for all age-groups except 16 to 20 and 75+ and for all racial and ethnic groups except for initial decreases among Hispanic males and NH Blacks followed by increases.
-
The largest annual increase occurred among NH White females.
-
Rates of acute alcohol-related deaths increased more for people aged 55 to 64, but rates of chronic alcohol-related deaths, which accounted for the majority of alcohol-related deaths, increased more for younger adults aged 25 to 34. (White et al., 2020)
Current low-risk drinking guidelines in the U.S. for healthy adults age 65 and under recommend no more than 4 drinks a day and no more than 14 drinks per week for men and no more than 3 drinks a day and no more than 7 drinks per week for women. (Women who are pregnant or may become pregnant should not drink any alcohol.) Sherk and colleagues (2020) evaluated the extent to which similar recommended low risk alcohol consumption guidelines in Canada served to reduce alcohol-related harms. The major conclusions and recommendation of this study were as follows:
-
Despite the comparatively high level of these guidelines, drinkers adhering to these limits were still exposed to increased hospital stays for both genders and increased mortality in men.
-
…even light or moderate alcohol consumption increased the risk for a number of health consequences, e.g., cancer, heart disease, digestive conditions, and traumatic injury.
-
More than one quarter (27%) of alcohol-caused hospital stays were experienced by people who drink within the weekly guidelines.
-
A gender neutral recommendation may be similar to that used in the Netherlands: don’t drink or, if you do, drink no more than one drink per day (International Alliance for Responsible Drinking, 2019).
Recent studies confirm the increase in alcohol-related deaths in the United States and that even drinking alcohol within recommended guidelines may result in untoward health consequences. These findings underscore the continued need for public alcohol-focused public/professional education, universal alcohol problems screening, alcohol-focused treatment resources, and sustained recovery support resources for individuals and families impacted by alcohol use disorders.
Alcohol and tobacco use is historically endemic in the United States. Such ritualized use is so infused into the cultural water in which we all swim that we fail to see it. That blindness has exacted, and continues to exact, an enormous toll on individuals, families, and communities.
References
White, A. M., Castle, I-J. P., Hingson, R. W., & Powell, P. A. (2020). Using death certificates to explore changes in alcohol-related mortality in the United States, 1999-2017. Alcoholism: Clinical and Experimental Research, 44 (1), 178-187.
Sherk, A., Thomas, G., Churchill, S., & Stockwell, T. (2020). Does drinking within low-risk guidelines prevent harm? Implications for high-income countries using the international model of alcohol harms policies. Journal of Studies on Alcohol and Drugs, 81, 352-361.

William White has a Master’s degree in Addiction Studies and has worked in outreach, clinical research and teaching roles in the addictions field since 1969. Bill has authored or co-authored more than 400 articles and 21 books, including Slaying the Dragon – The History of Addiction Treatment and Recovery in America and, more recently, Recovery Rising.
To date, eleven articles authored or co-authored by Bill have been posted on AA Agnostica. Here are the previous ones, in order:
Recovery is Contagious (July 07, 2019)
Recovery Spirituality (January 20, 2019)
Addiction, Recovery, and Personal Character (June 14, 2018)
The Secular Wing of AA (March 04, 2018)
The Karma of Recovery (January 04, 2018)
Recovery Pathways are not always a Pathway (December 21, 2017)
AA Agnostica and the Varieties of AA Experience (August 03, 2014)
The Resilience of Alcoholics Anonymous (June 01, 2014)
Agnostic Groups in AA – An Interview (March 17, 2013)
A Message of Tolerance and Celebration (December 30, 2012)
The post Alcohol: A Hidden Epidemic? first appeared on AA Agnostica.


![Do Tell! [Front Cover]](https://nrdblogs.nationalrehabdirectory.net/wp-content/uploads/2020/09/Do-Tell-Full-Blue-Front-Cover-200-FRAMED.jpg)

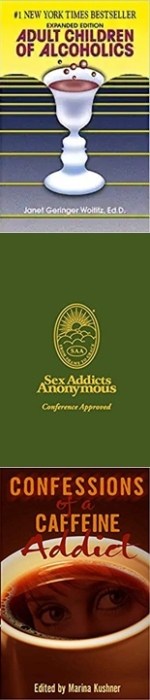
 The clarity of sobriety made me realize, David, you have other obsessive/addictive issues. Father was an alcoholic? Try Adult Children of Alcoholics. Trauma based sexual dysfunction? Perhaps Sex Addicts Anonymous would help. Coffee addiction? Check out Caffeine Addicts Anonymous. Even though narcotics are not a personal issue for me, detox and an in-patient facility exposed me to Narcotic’s and Cocaine Anonymous meetings and literature.
The clarity of sobriety made me realize, David, you have other obsessive/addictive issues. Father was an alcoholic? Try Adult Children of Alcoholics. Trauma based sexual dysfunction? Perhaps Sex Addicts Anonymous would help. Coffee addiction? Check out Caffeine Addicts Anonymous. Even though narcotics are not a personal issue for me, detox and an in-patient facility exposed me to Narcotic’s and Cocaine Anonymous meetings and literature.